- Visibility 202 Views
- Downloads 24 Downloads
- DOI 10.18231/j.jooo.2020.013
-
CrossMark
- Citation
Diagonosis of dental caries: A conventional and current perspective
- Author Details:
-
Saman Ishrat
-
Akhilanand Chaurasia *
Introduction
Caries diagnosis has been defined as “the art or act of identifying a disease from its signs and symptoms” and caries detection is the signs and symptoms identified.[1] There is often confusion in the literature in the terminology used for caries detection and caries diagnosis. In the last decade, three terms have been agreed in terms of direct relevance to preventive caries care,[2] lesion detection: implies an objective method of determining whether or not disease is present,[3] lesion assessment: aims to characterize or monitor a lesion once it has been detected[4] and caries diagnosis: should imply a human, professional, summation of all available data.[5] The continuous process of caries has been represented by an iceberg as a metaphor to conceptualize dental caries. The iceberg represents the whole arrange of lesions and shows how traditional methods may leave undetected a large number of early lesions depending at which diagnostic threshold the methods are used.[6]

The Visual-tactile Examination
Proximal caries has in particular proven to be very difficult to diagnose using the visual tactile method, as 83% of cavitated proximal caries lesions were not detected using this method alone.[7] In regards to this, the site-specific gingival scores seem to correlate with the presence of cavitated proximal lesions. This might be due to the fact that cavitated lesions retain plaque and food debris, which can cause inflammation of the gingiva. Gingival inflammation could thus be used as an additional diagnostic indicator for the presence or absence of cavitation.[7]
Caries diagnosis based on a visual-tactile examination alone is difficult, and misclassifications occur to a greater extent among non-cavitated lesions than cavitated ones.[8] Concerning occlusal caries, it seems that the probe is not a reliable method for the detection of caries. Even worse, the probe may sometimes actually cause cavities in the search for caries.[8] The probe is, very carefully used, still a suitable tool for the assessment of root caries, as the texture of the root surface is the main diagnostic criteria for caries, not the color.[9]

Dental Radiography
Dental radiography is electromagnetic radiation, which has wavelengths between 0.01 to 10 nanometers. It is a useful diagnostic method which utilizes the fact that the absorption of the x-rays differs depending on what type of tissue they penetrate. The difference can be visualized by the use of different kind of detectors, analog, as well as digital. X-ray is especially useful for hard tissue diagnostics. Unlike the visual-tactile method, X-rays are potentially harmful, and should only be used when indicated.
Radiographs are useful for caries detection because caries causes demineralization of the tooth structure. Demineralized tooth structure attenuates the x-ray photons to a lesser extent than sound tooth structure. A minimum of 60% demineralization must occur before the lesion can be seen on a film-based radiograph. Digital radiographs are in the 50-55% range.
Which radiographs are best for caries detection?
Bitewing projections provide optimal visualization of proximal and occlusal caries in the posterior teeth. Periapicals are appropriate for anterior proximal caries. Paralleling technique improves visibility of the lesion. Occlusal caries can often be detected on panoramic projections. As always, aligning instruments are mandatory for optimal results. Since carious lesions often have low contrast with surrounding healthy tissue, optimal viewing conditions are imperative. In the context of caries detection, X-ray is a useful tool, but should not be used as the sole diagnostic tool. This is especially true for the detection of occlusal caries, which is the most prevalent form of caries in the population.[10] Proximal dentin lesions are, however, more easily detected with X-ray compared to the visual-tactile method. Combining the visual-tactile method with bitewing radiographs seems to yield higher sensitivity and specificity, compared to either method alone.[8]


Laser Diagnostics
Dental laser diagnostic is a non-ionizing diagnostic method based on the measurement of the fluorescence of the enamel and dentin. Demineralized enamel has different optical attributes compared to the healthy enamel. Demineralized enamel can visually be seen as a white spot lesion. The optical change is caused by increased pore volume in the demineralized enamel. This change of the optical values can be quantified by a laser fluorescence device and theoretically it can be used to identify early caries lesions. The LF device consists of 655 nm monochromatic light that is emitted from a tip/sensor and can detect back-scattered fluorescence from the tooth.[11] At 655 nm, the fluorophores have been identified as bacterial porphyrins. The DD scores ranges between 0 and 99. This number offers the possibility to monitor lesion behavior.[12] An example of such a device is the Kavo DIAGNO dent. It is a small chairside battery powered laser fluorescence device. It is used by scanning the area of interest and noting the peak value that the device shows. The value can then be interpreted to decide whether treatment is needed. The values will vary depending on age, tooth color, staining, and location of lesions. The recommended cut-off value that yields the highest sensitivity and specificity can be found in scientific literature.[13] The Kavo DIAGNOdent method shows a very high sensitivity for low cut-off values. Cut-off values are the baseline for which higher values will be interpreted as the presence of caries lesions. Unfortunately the specificity is poor for low values.[14] This may be caused by calculus, fillings and/or stain that will give an artificial high value, which can be interpreted as caries.
Studies do however report excellent intra-examinator reliability and good to excellent interexaminator reliability by using the Kavo DIAGNOdent, i.e. getting a correct value does not seem to be affected by experience. However, the type of carious lesions (proximal/occlusal) and different kinds of tooth surfaces will also affect the values.[15] KaVo DIAGNOdent is a viable tool for the diagnosis of occlusal dentin caries, and studies even suggest that the KaVo DIAGNOdent combined with the visual-tactile method is a superior diagnostic option for the diagnosis of fissure caries, compared to the visual-tactile method supplemented with radiographs.[16] The KaVo DIAGNOdent is also a useful diagnostic tool, in combination with the visual-tactile method, for detection of proximal lesions. Accurate results have however been difficult to obtain in cases of tight contact points, due to the large tip of the tool. A smaller tip is suggested to help aid better diagnostics.[13] When it comes to the detection of early caries lesions, the reports are more mixed. According to one study,[13] the KaVo DIAGNOdent could differentiate between caries up to the EDJ and dentin caries in proximal lesions by a sensitivity of 0,6 and a specificity of 0,84 given a cutoff value of 16. This implies that there is no significant difference between dental radiographs and the KaVo DIAGNOdent when it comes to the diagnosis of early proximal caries lesions in permanent teeth.[13]


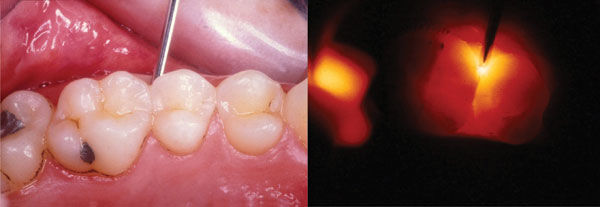
Fiber-optic trans Illumination
Fiber-optic Trans illumination (FOTI) is a diagnostic tool for the detection of caries which utilizes the fact that caries can change the optical properties of the tooth substance. These optical changes can be seen as shadows, which can be interpreted as caries. No studies solely concerned with FOTI were found, but a paper evaluating FOTI was mentioned by Huth KC et al. (2010).[13] In this study, FOTI was described as the least reliable method for caries detection considered in that specific paper. Elective temporary tooth separation detected 41.4% more lesions compared to FOTI, and revealed that 17.5% of the lesions diagnosed by FOTI were actually sound enamel when clinically assessed.[17]
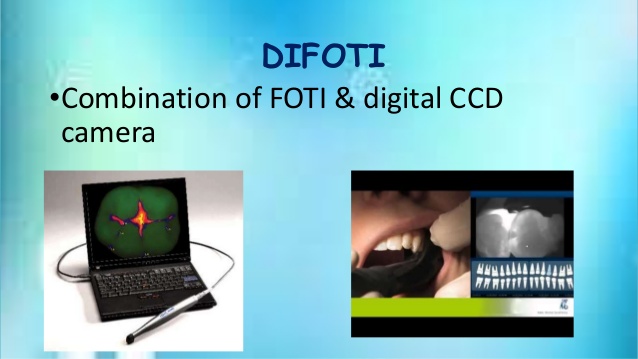
In a recent review, only three in vitro studies reported findings for NCCLs using FOTI.[18], [19], [20] The Sensitivity scores for FOTI ranged from 0.21 to 0.96, and the Specificity ranged from 0.74 to 0.88.[21] DIFOTI (Digital Fibre-optic Transillumination) replace the human eye with a CCD sensor. The transillumination method may support a treatment decision-making but it is not able of monitoring dental caries lesions as the bitewing radiographs.[22] Recent developments in ordinal scales for visual assessments, such as the ICDAS scoring system may enable a more robust framework for visual exams into which FOTI can be added.[23]
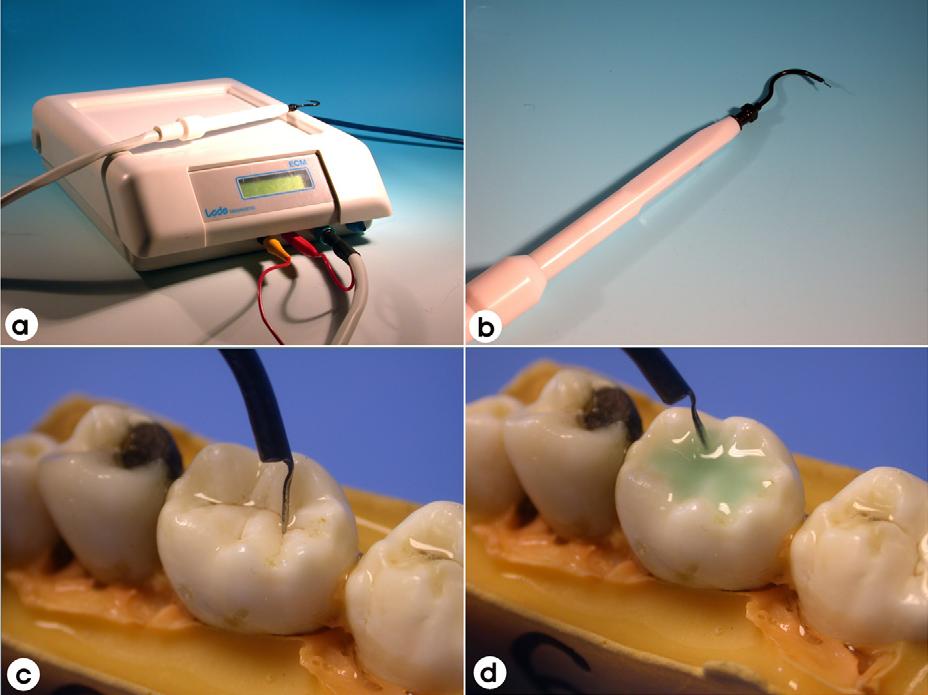
Electric Caries Monitor (ECM)
Demineralisation, in theory, creates porosities; the porosities will fill with water and ions from saliva causing electrical conductivity changes.[24] The ECM device employs a single, fixed-frequency alternating current, which attempts to measure the ‘bulk resistance’ of tooth tissue.[25] The degree of electrical conductance is dictated by the properties of the substance including porosity, the contact area, the thickness of the tissue, hydration of the enamel, and ionic content of dental fluids.[26] The method has shown promising results showing superior performance to FOTI and radiography in early lesions.[21] However, previous studies have shown the presence of stain as a confounder factor.[20] Another issue is the wide variations on reproducibility, possibly due to inconsistent probe contact with the tooth surface.[27]
QLF (Quantitative light-induced fluorescence)
QLF is a diagnostic aid for detection, quantification and monitoring of early enamel demineralisation. QLF operates on the principle of enamel autofluorescence, detecting and quantifying the loss of fluorescence associated with demineralization.[23] The technique is based on the principle of the excitation of the dentine with blue light (370 nm) and would make it to fluoresce into yellow-green region. When a lesion is present, an increase of light scattering makes appear the lesion as dark spots on a bright green background. The loss of fluorescence images can be quantified with respect to adjacent healthy tissue.[28] The fluorescent image of the tooth is recorded and digitalised and analysed quantitatively. The loss of fluorescence is obtained by reconstruction of the fluorescence of healthy enamel, assuming that is 100%. The decrease in fluorescence is determined by calculating the percentage difference between the actual and the reconstructed surface. Any area with a decrease in fluorescence over 5% is considered as a lesion.[29] The reliability of the QLF in vivo appears to be excellent for the quantification of initial caries lesions on smooth surfaces.[29] QLF has shown good sensitivity in vivo.[30] However, the specificity is sometimes compromised due to the confounding factors. Correlations of up to 0.82 have also been reported for QLF metrics and lesion depth.[23] QLF has also shown the ability to detect and quantify changes of mineral content and size of lesions by demonstrating a dose response between F and non-F dentifrices in short-term clinical trials.[31], [32]

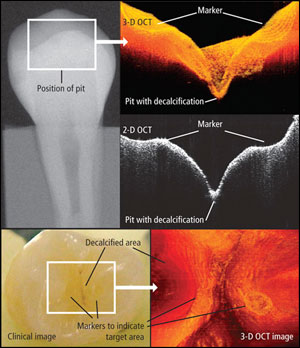
Optical Coherence Tomography (OCT)
OCT is a high-resolution, non-invasive imaging technique that constructs crosssectional images of internal biological structures.[33] This technology is based on the principle of optical interferometry using a low coherence light source that is split into two beams, which then are reflected back, one from the investigated tissue and the other from a reference mirror, and combined together to create an interference pattern that contains depth-information from the sample.[34] The OCT system used a wavelength of 850 - 1310 nm resulting in image depths of 0.6-2.0 mm. Previous studies have shown that OCT has the potential to detect and quantify demineralisation based on an increase light scattering from porous structures within the tooth in in vitro caries-like models.[34], [35] However, in vitro models did not reflect the complexity of natural lesions; in particular they were not subsurface lesions.[35] Previous studies have shown the potential use of OCT to detect and quantify demineralisation based on an increase light scattering from porous structures within the relatively new, there is still much work to be done to assess its full potential.
Midwest Caries I.D.
The Midwest Caries I.D. detects differences of optical behavior inside the tooth related to change in the tooth structure and it is therefore not sensitive to bacterial content. The Midwest Caries I.D. uses infrared and red light emitting diodes LEDs and a fiber optic to distribute light to the observed area present at the probe tip. A second fiber optic collects light from the observed area to a photodetector that measures returned collected light. This photodetector then transmits the signal to a microprocessor that compares signal levels with defined parameters. When the result is positive, the processor deactivates the third green LED and pulses at a higher intensity than the red LED. When the detection is negative i.e., healthy tooth area, the green LED is dominant resulting in a green illumination when healthy structure is detected and red illumination when caries are detected. A buzzer also beeps with different frequencies to indicate the intensity of demineralization detected. The Midwest Caries I.D. can be used for approximal caries detection during the examination by slightly angling and moving the probe along the marginal ridge just over the vulnerable approximal area. This approach seems much more convenient than the DIAGNOdent approach since it enables minimal dilution of the light signal from all surrounding structures _which is the case for transillumination_ by sending and capturing the light signal in a direct line toward the vulnerable regions inside the enamel.[36] One of the few studies evaluating this device reported the sensitivity and specificity to be higher than that of DIAGNOdent.[36] Interproximal detection using the Midwest Caries I.D. and x rays as a gold standard showed a sensitivity of 80% and specificity of 98%.[37] However, this device can give false positive signals in cases of teeth with growth malformations in the enamel or the dentin, teeth with thick, dark stains, hypermineralization, hypocalcification, dental fluorosis, and atypically shaped teeth due to alteration in the translucency of enamel caused by these conditions.[38] Light penetration is limited into the enamel and up to 3 mm in approximal area. Midwest Caries I.D. cannot be used on composites or amalgams but can be used to check the marginal ridges of occlusal amalgams. If the probe is tipped at too much of an angle when checking for approximal caries, total surface light reflection can occur giving a false positive. Opaque artifacts plaque, calculus and organic plug can cause false positives. [36]

CarieScan
This device is based on the proven technology of alternating current impedance spectroscopy and involves the passing of an insensitive level of electrical current through the tooth to identify the presence and location of the decay. The frequency domain is based on a sinusoidal signal applied to a sample at known amplitude and frequency. The response waveform is then measured and the impedance calculated by a transfer function relationship of the applied voltage perturbation and acquired response current. It is the first dental diagnostic tool to use ac impedance spectroscopy to quantify dental caries early enough to enhance preventative treatment. According to the originators[38] the CarieScan is not affected by optical factors such as staining or discoloration of the tooth; it provides a qualitative value based on the disease state rather than the optical properties of the tooth. The device is indicated for the detection, diagnosis, and monitoring of primary coronal dental caries occlusal and accessible smooth surfaces, which are not clearly visible to the human eye. It cannot be used to assess secondary caries, the integrity of a restoration, dental root caries, and the depth of an excavation within a cavity preparation. This device uses disposable tufted sensors for single use and a test sensor nondisposable, which is used to test the device and confirm if the system is operating correctly. For assessment of caries, while tufted sensor brush contacts the tooth surface being examined, a soft tissue contact, which is a disposable metal clip that is placed over the lip in the corner of the patient’s mouth, connects to the CarieScan via a soft tissue cable to complete the circuit. During measurement, a green color display indicates sound tooth tissue, while a red color indicates deep caries requiring operative, and a yellow color associated with a range of numerical figures from 1 to 99 depicts varying severity caries, which require only preventive care. Accompanying the CarieScan is the CarieScan-Plus, which is a wirelessly linked control system designed to be used as a patient management system, allowing data to be automatically captured, filed, and recalled electronically on a bytooth, by-surface, by-date basis for dental health monitoring. This enhances communication with the patient as an aid to preventive motivation and caries control. A systematic review[39] comparing CarieScan with clinical visual examination, bitewing radiograph, and DIAGNOdent reported CarieScan to have a superior sensitivity and specificity both 92.5% over other methods.

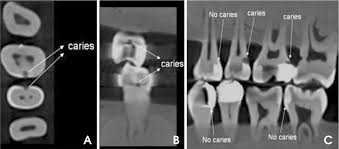
Cone Beam Computed Tomography
The application of cone beam computed tomography CBCT in dental caries diagnosis has not been widely studied. The first and only study[40] that compared caries diagnosis ability of two CBCT systems, NewTom 3G Quantitative Radiology and 3DX Accuitomo, and two intraoral modalities, Digora-fmx Soredex and film Kodak Insight, with histological technique serving as the validation standard concluded that the NewTom 3G CBCT had a lower diagnostic accuracy for detection of caries lesions than intraoral modalities and the 3DX Accuitomo CBCT. The Accuitomo CBCT had a higher sensitivity than the intraoral systems for detection of lesions in dentin, but the overall true score was not higher.[40] The investigation to apply in caries diagnosis stems from its numerous advantages when compared to all current forms of x-ray imaging. CBCT utilizes the least amount of radiation to obtain a diagnostic image while remaining cost effective for patients.[41] By comparison, the NewTom® 3G generates an average CBCT study using 12.0 Sv. This radiation dose is similar to a quarter panoramic image or five dental x rays using high-speed film.105 Because less radiation means less exposure time, the complete cycle to make one slice by the NewTom® 3G takes 36s, while the actual exposure time to the patient is 5.6s.[41] By comparison, a panoramic image requires 20–100 Sv. CBCT scanners are more accurate than dental periapical films or panoramic x rays. While there is clearly less radiation used to generate a panoramic image, the amount of information it renders is less accurate and not as useful when compared to the three-dimensional images of a CBCT scan.[42]
Frequency-domain Infrared Photothermal Radiometry and Modulated Luminescence
Although still under development, the most recent technology in the field of caries diagnosis is the combined frequency-domain laser-induced infrared photothermal radiometry and modulated luminescence PTR/LUM. Some of the inherent advantages of the adaptation of PTR to dental diagnosis in conjunction with LUM emission as the dualprobe technique have been reported in recent literature.[43], [44], [45], [46], [47] The PTR technique is based on the modulated thermal infrared blackbody or Planck radiation response of a medium, resulting from optical radiation absorption from a lowintensity laser beam and optical-to-thermal energy conversion followed by modulated temperature rise “thermal waves” usually less than 1 °C in magnitude. The generated signals from PTR/LUM instrument carry subsurface information in the form of a spatially damped temperature.[39] Thus PTR has depth-profilometric ability i.e it can penetrate and yield information about an opaque or highly scattering medium well beyond the range of optical imaging. The laser-intensity modulation-frequency dependence of the penetration depth of thermal waves makes it possible to perform depth profiling of materials.
Source of Funding
None.
Conflict of Interest
None.
References
- B. Nyvad. Diagnosis versus Detection of Caries. Caries Res 2004. [Google Scholar]
- P E Petersen, D Bourgeois, H Ogawa, S Estupinan-Day, C Ndiaye. The global burden of oral diseases and risks to oral health. Bull World Health Organ 2005. [Google Scholar]
- R.P. Ellwood, J. Goma, I.A. Pretty. Caries Clinical Trial Methods for the Assessment of Oral Care Products in the 21st Century. Adv Dent Res 2012. [Google Scholar]
- T M Marthaler. The Caries-Inhibiting Effect of Amine Fluoride Dentifrices in Children during Three Years of Unsupervised Use. Br Dent J 1965. [Google Scholar]
- N.B. Pitts, J.W. Stamm. International Consensus Workshop on Caries Clinical Trials (ICW-CCT)—Final Consensus Statements: Agreeing Where the Evidence Leads. J Dent Res 2004. [Google Scholar]
- N B Pitts. Modern concepts of caries measurement. J Dent 2004. [Google Scholar]
- D K Ratledge. A clinical and microbiological study of approximal carious lesions. Part 1: the relationship between cavitation, radiographic lesion depth, the site-specific gingival index and the level of infection of the dentine. Caries Res 2001. [Google Scholar]
- J A Rodrigues. Prevention of crown and root caries in adults. Periodontol 2000. [Google Scholar]
- M Brazzelli, L McKenzie, S Fielding, C Fraser, J Clarkson, M Kilonzo. Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries. Health Technol Assess 2006. [Google Scholar] [Crossref]
- D N Ricketts, E A Kidd, D Beighton. Operative and microbiological validation of visual, radiographic and electronic diagnosis of occlusal caries in non-cavitated teeth judged to be in need of operative care. Br Dent J 1995. [Google Scholar]
- A. Lussi, S. Imwinkelried, N.B. Pitts, C. Longbottom, E. Reich. Performance and Reproducibility of a Laser Fluorescence System for Detection of Occlusal Caries in vitro. Caries Res 1999. [Google Scholar]
- K W Neuhaus, C Longbottom, R Ellwood, A Lussi. Novel lesion detection aids. Monogr Oral Sci 2009. [Google Scholar]
- K C Huth. 2010 -In vivo performance of a laser fluorescence device for the approximal detection of caries in permanent molars. J Dent 2010. [Google Scholar]
- C H Chu. Clinical diagnosis of fissure caries with conventional and laser-induced fluorescence techniques. Lasers Med Sci 2010. [Google Scholar]
- K C Huth. Clinical performance of a new laser fluorescence device for detection of occlusal caries lesions in permanent molars. J Dent 2008. [Google Scholar]
- J A Rodrigues. Prevention of crown and root caries in adults. Periodontol 2000. [Google Scholar]
- C Deery. Prevalence of Dental caries in Latvian 11- to 15-year-old children and the enhanced diagnostic yield of temporary tooth separation, FOTI and electronic caries measurement (Reference found in Huth KC et al - 2010). Caries Res 2000. [Google Scholar]
- P.F. Ashley, A.S. Blinkhorn, R.M. Davies. Occlusal caries diagnosis: an in vitro histological validation of the electronic caries monitor (ECM) and other methods. J Dent 1998. [Google Scholar]
- D.F. Côrtes, K.R. Ekstrand, A.R. Elias-Boneta, R.P. Ellwood. An in vitro Comparison of the Ability of Fibre–Optic Transillumination, Visual Inspection and Radiographs to Detect Occlusal Caries and Evaluate Lesion Depth. Caries Res 2000. [Google Scholar]
- D.F. Côrtes, R.P. Ellwood, K.R. Ekstrand. An in vitro Comparison of a Combined FOTI/Visual Examination of Occlusal Caries with Other Caries Diagnostic Methods and the Effect of Stain on Their Diagnostic Performance. Caries Res 2003. [Google Scholar]
- Juliana Gomez, M. Tellez, I.A. Pretty, R.P. Ellwood, A.I. Ismail. Non-cavitated carious lesions detection methods: a systematic review. Community Dent Oral Epidemiol 2013. [Google Scholar]
- K W Neuhaus, R Ellwood, A Lussi, N B Pitts. Traditional lesion detection aids. Monogr Oral Sci 2009. [Google Scholar]
- Iain A. Pretty. Caries detection and diagnosis: Novel technologies. J Dent 2006. [Google Scholar]
- D N Ricketts, E A Kidd, P J Liepins, R F Wilson. Histological validation of electrical resistance measurements in the diagnosis of occlusal caries. Caries Res 1996. [Google Scholar]
- C. Longbottom, M.-C.D.N.J.M. Huysmans. Electrical Measurements for Use in Caries Clinical Trials. J Dent Res 2004. [Google Scholar]
- K W Neuhaus, C Longbottom, R Ellwood, A Lussi. Novel lesion detection aids. Monogr Oral Sci 2009. [Google Scholar]
- M.-C.D.N.J.M. Huysmans, C. Longbottom. The Challenges of Validating Diagnostic Methods and Selecting Appropriate Gold Standards. J Dent Res 2004. [Google Scholar]
- M H Van Der Veen, E De Josselin De Jong. Application of quantitative lightinduced fluorescence for assessing early caries lesions. Monogr Oral Sci 2000. [Google Scholar]
- E. de Josselin de Jong, F. Sundström, H. Westerling, S. Tranaeus, J.J. Ten Bosch, B. Angmar-Månsson. A New Method for in vivo Quantification of Changes in Initial Enamel Caries with Laser Fluorescence. Caries Res 1995. [Google Scholar]
- A. Ferreira Zandoná, E. Santiago, G. Eckert, M. Fontana, M. Ando, D.T. Zero. Use of ICDAS Combined with Quantitative Light-Induced Fluorescence as a Caries Detection Method. Caries Res 2010. [Google Scholar]
- S Tranaeus, S Al-Khateeb, S Bjorkman, S Twetman, B Angmar-Mansson. Application of quantitative light-induced fluorescence to monitor incipient lesions in caries-active children. A comparative study of remineralisation by fluoride varnish and professional cleaning. Eur J Oral Sci 2001. [Google Scholar]
- Y. Feng, W. Yin, D. Hu, Y.P. Zhang, R.P. Ellwood, I.A. Pretty. Assessment of Autofluorescence to Detect the Remineralization Capabilities of Sodium Fluoride, Monofluorophosphate and Non-Fluoride Dentifrices. Caries Res 2007. [Google Scholar]
- D Huang, E A Swanson, C P Lin, J S Schuman, W G Stinson, W Chang. Optical coherence tomography. Sci 1991. [Google Scholar]
- R.S. Jones, C.L. Darling, J.D.B. Featherstone, D. Fried. Imaging Artificial Caries on the Occlusal Surfaces with Polarization-Sensitive Optical Coherence Tomography. Caries Res 2006. [Google Scholar]
- Hobin Kang, J J Jiao, Chulsung Lee, M H Le, C L Darling, D L Fried. Nondestructive Assessment of Early Tooth Demineralization Using Cross-Polarization Optical Coherence Tomography. IEEE J Sel Top Quantum Electron 2010. [Google Scholar]
- H Ciaburro, D M D Krause. Occlusal caries detection in posterior teeth: An in vivo comparison of D-Carie and DIAGNOdent, sponsored study by NEKS Technologies. . [Google Scholar]
- F Martel. Interproximal caries detection: An in vivo comparison of D-Carie with x rays, sponsored study by NEKS Technologies. . [Google Scholar]
- James D. Bader, Daniel A. Shugars, Arthur J. Bonito. Systematic Reviews of Selected Dental Caries Diagnostic and Management Methods. J Dent Educ 2001. [Google Scholar]
- Alan A Winter, Alan S Pollack, Herbert H Frommer, Lisa Koenig. Cone Beam Volumetric Tomography vs. Medical CT Scanners. N Y State Dent J 2005. [Google Scholar]
- M Sonick, J Abrahams, R Faiella. A Comparison of the Accuracy of Periapical, Panoramic, and Computerized Tomographic Radiographs in Locating the Mandibular Canal. Int J Oral Maxillofac Implants 1994. [Google Scholar]
- Lena Nicolaides, Andreas Mandelis, Stephen H. Abrams. Novel dental dynamic depth profilometric imaging using simultaneous frequency-domain infrared photothermal radiometry and laser luminescence. J Biomed Opt 2000. [Google Scholar]
- A Mandelis. Proc. SPIE 4710. 2002. [Google Scholar]
- R J Jeon, C Han, A Mandelis, V Sanchez, S H Abrams. Diagnosis of Pit and Fissure Caries Using Frequency-Domain Infrared Photothermal Radiometry and Modulated Laser Luminescence. 2004. [Google Scholar]
- Raymond J. Jeon, Andreas Mandelis, Victor Sanchez, Stephen H. Abrams. Nonintrusive, noncontacting frequency-domain photothermal radiometry and luminescence depth profilometry of carious and artificial subsurface lesions in human teeth. J Biomed Opt 2004. [Google Scholar]
- R J Jeon, A Matvienko, A Mandelis, S H Abrams, B T Amaechi. Detection of Interproximal Demineralized Lesions on Human Teeth in Vitro Using Frequency-Domain Infrared Photothermal Radiometry and Modulated Luminescence. J Biomed Opt 2007. [Google Scholar]
- M Munidasa, A Mandelis. Photothermal and Photoacoustic Science and Technology, Photothermal Imaging and Microscopy Vol. I, edited by A. Mandelis Society for Optical Engineering SPIE. 1992. [Google Scholar]
- Introduction
- The Visual-tactile Examination
- Dental Radiography
- Laser Diagnostics
- Fiber-optic trans Illumination
- Electric Caries Monitor (ECM)
- QLF (Quantitative light-induced fluorescence)
- Optical Coherence Tomography (OCT)
- Midwest Caries I.D.
- CarieScan
- Cone Beam Computed Tomography
- Frequency-domain Infrared Photothermal Radiometry and Modulated Luminescence
- Source of Funding
- Conflict of Interest
