- Visibility 81 Views
- Downloads 10 Downloads
- DOI 10.18231/j.jooo.2020.020
-
CrossMark
- Citation
Duplication of recurrent laryngeal nerve in thyroid surgery – a rare anatomical variation
- Author Details:
-
Chinmaya Sundar Ray
-
Krishna Arpita Sahoo *
Introduction
Injury to the recurrent laryngeal nerve is one of the most serious complications after thyroid surgery leading to vocal cord paralysis.[1] When it is bilateral, induces major respiratory consequences requiring tracheostomy or segmental posterior cordectomy. Surgeons must have a comprehensive understanding of the anatomy of RLN during thyroid operation. There are several anatomical variations of nerve ranging from extra-laryngeal branches, distorted pattern, intertwining between branches of the recurrent laryngeal nerve and the inferior thyroid artery & non-recurrent laryngeal nerve which might increase the risk of iatrogenic damage.[2], [3] There is possibility of abnormal branches and duplication of nerves though uncommon should not be underestimated and extra vigilance must be exercised when operating near a nerve. Routine identification of recurrent laryngeal nerve during thyroidectomy reduces the rate of injury. It can be further confirmed with nerve monitors.[4] The average incidence of temporary postoperative vocal fold palsy is around 3-8% and incidence of permanent RLN injury is 2.3%.[5] The rate of intra-operative injury to nerve can be decreased dramatically with intra-operative neuro-monitoring.
Case Report
Case 1
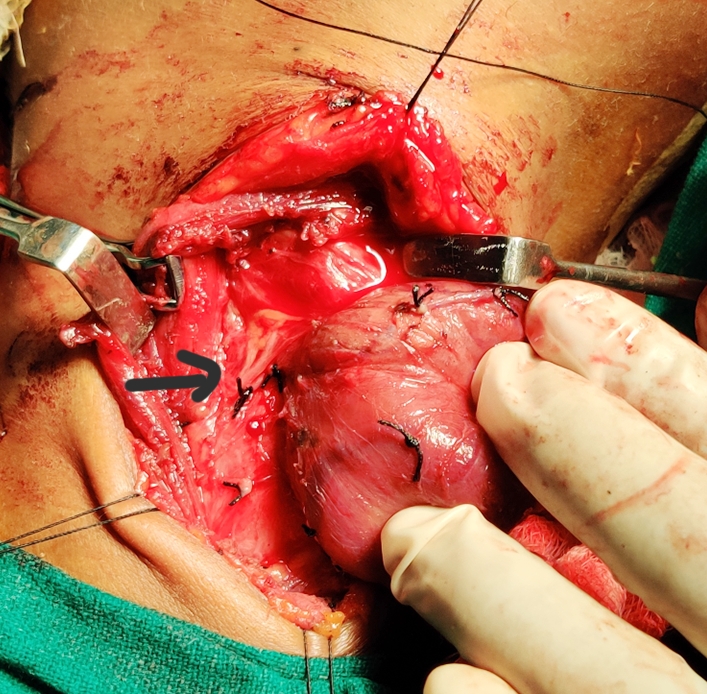
A 45-year-old lady presented with a firm and mobile neck swelling since 1 year. The swelling was painless but slowly and progressively increasing in size. The swelling moved on deglutition. On examination, the size of thyroid swelling was approximately 6×4 cm on the right side. On ultrasongrapy, it revealed a 54x38 mm benign nodule of right lobe with colloid material which was iso-echoic relative to the thyroid and surrounded by hypo-echogenic halo. Fine needle aspiration cytology suggested it to be a colloid goiter, benign in origin. She had no history of surgery or exposure of radiation to head & neck. Preoperative assessment including thyroid hormone profile was normal and the patient was taken for surgery under general anaesthesia. Patient underwent hemithyroidectomy on right side. During the surgery, it was found that there was duplication of the right recurrent laryngeal nerve. Intraoperatively, we confirmed it with the nerve monitor followed by careful dissection of the branch to prevent injuries. The nerve on the right was smaller and displaced laterally by the goiter, whereas the other was adjacent to the trachea and behind the goiter. Both nerves separately exited at the level of cricothyroid joint before innervating the larynx. The postoperative period was uneventful and follow-up assessments revealed no signs of nerve injury like hoarseness of voice.
Case 2
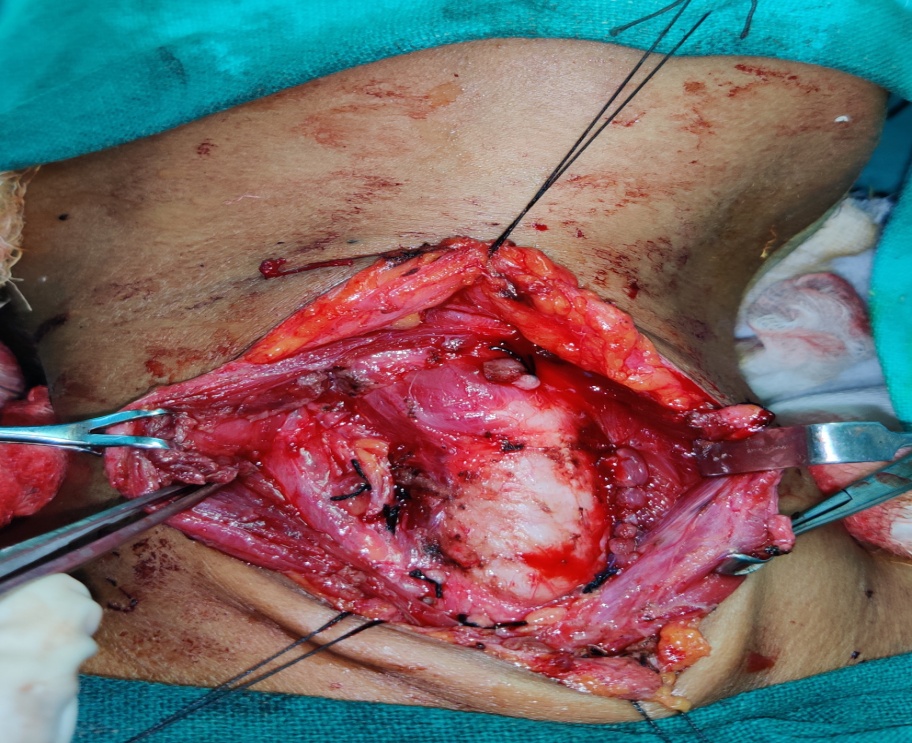
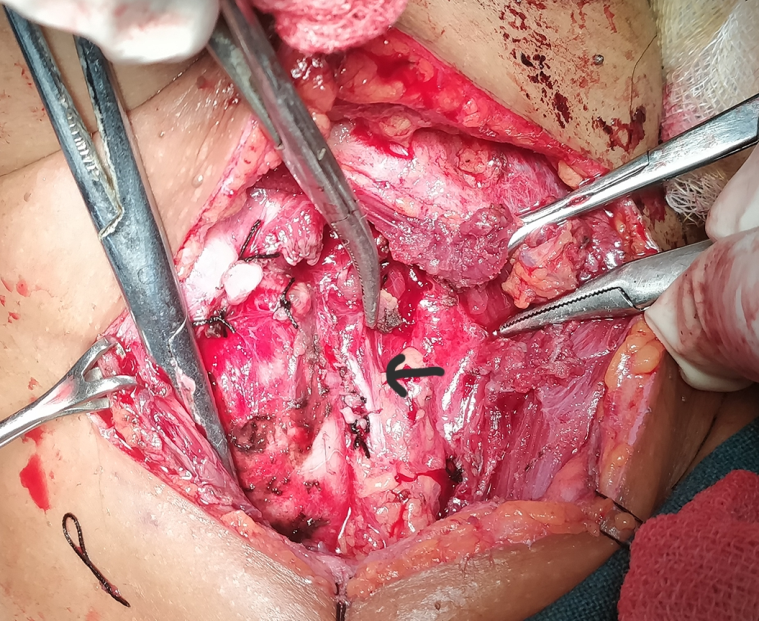
A 55-year old female patient with large size goiter underwent total thyroidectomy. Fine needle aspiration cytology recorded it to be papillary carcinoma. Ultrasonography revealed the size to be 42x 34 mm and with microcalcifications. Pre-operative assessment revealed normal thyroid profile with no signs of vocal cord paralysis. Intra-operatively, after ligating the inferior thyroid vessels on left side we identified the recurrent laryngeal nerve in the trachea-esophageal groove. While further dissecting on the same side, a thread like structure was present lateral to the identified recurrent laryngeal nerve. It was mistaken as a vessel and was slightly thinner than the original nerve. On further dissection cranially till the cricothyroid joint, we could find that it was a separate branch of the left recurrent laryngeal nerve. The nerve along with its branch was preserved till the entrance of the larynx. But there was no bifurcation of nerve when we proceeded caudally. A single recurrent laryngeal nerve was present on the right side. On histopathological study, it was diagnosed as a case of papillary carcinoma of thyroid gland. Post-operatively, on laryngoscopy there was normal movement of vocal cords. The patient received radio-iodine therapy 6 weeks after surgery along with thyroid hormone replacement therapy, calcium, iron and vitamin D3 supplements.
Discussion
The RLN was first described by Galen in the second century AD. The RLN was the principal nerve which controlled vocal fold movement through its laryngeal branches.[6] The nerve consists of motor, sensory and autonomic fibres. It branches from the vagus nerve in the superior part of the thorax, on the right at the level of right subclavian artery and on the left side at the level of the arch of the aorta. The right RLN is about 7 cm long and left is around 12 cm between its origin in vagus nerve & entrance into larynx. RLN may cross above or below the inferior thyroid artery, or between its branches.
Visual identification of the RLN& systematic dissection is mandatory during thyroid surgery to prevent nerve injury. Injury to the RLN after thyroid operations is one of the most serious complications that is the reason for medico-legal litigation. Intra-operative nerve monitoring (IONM) is the modern surgical strategy for identifying the anatomy of the RLN and its variants during surgical dissection.[7] In revision surgeries, IONM seems to be more useful for making the functional integrity of the nerve.
Anatomic variations of the RLN represent a major threat to nerve injury. In two of the present cases during thyroidectomy RLN bifurcates before it enters larynx at the level of crico-thyroid joint. During surgery, a few anatomic landmarks can help in identification of the nerves. The Tubercle of Zuckerkandl marks the posterolateral aspect of the thyroid lobe and is most often found lateral to the recurrent laryngeal nerve. Most often, the nerve is found in a groove between the tubercle and the lobe of the thyroid gland. Additionally, Berry’s ligament can be used for identification, since the nerves are found in close proximity to the ligament. The commonest area to identify both the right & left inferior laryngeal nerve is near the lower pole where it courses close to the inferior thyroid artery at the middle or lower third of the posterolateral surface of the thyroid lobe.[8] Identification of nerve can be from a superior-to-inferior approach (from its insertion into the larynx) or an inferior-to-superior approach (identification at the inferior pole) as proposed by Veyseller et al. It is found that a lower rate of hypoparathyroidism using the superior-to-inferior approach for identifying the RLN. However, every approach depends on both surgeon preference and the indication for the thyroidectomy.
The recurrent laryngeal nerve is known to have about 30 anatomical variations. Due to these variations, the risk of nerve injury during surgery is reported to be 1–2% even in experienced hands. These include the variable course of the RLN at the level of the inferior thyroid artery, the relationship between the RLN and posterior tubercle (Zuckerkandl’s tubercle), non-recurrent laryngeal nerves (NRLN), and extralaryngeal bifurcation. About 0.3–0.8% the right RLN does not recur, and originates from the cervical portion of the vagus nerve. It has been found that non-recurrence of the right inferior laryngeal nerve results from a vascular anomaly during the embryonic of the aortic arches. Non-recurrent laryngeal nerve is usually an incidental finding, with a risk of intra-operative nerve injury.[9] Branching of nerve or duplications is seen in 30-76% cases before entering the larynx at the level of berry’s ligament. The recurrent laryngeal nerve gives off 2–8 branches that are asymmetric at the right and left sides. It has been reported that the rates of a single main branch as 0–65.8%, two branches as 52–94%, three branches as 0.8–48%, four branches as 0–25%, and five branches as 0–10% Nemiroff et al. reported the branching distance as approximately 0.6 to 4 cm from the lower border of the cricoid cartilage. Most of the duplications of RLNs have two branches: the anterior (motor branch) and posterior (sensory branch).[10], [11] The discovery of an abnormally thin nerve must alert the surgeon to the possibility of a second branch coursing towards the larynx. Variations exist where the branches of the inferior thyroid artery can be anterior or posterior to the nerve, or the nerve can run in between the branches of the artery. The right recurrent laryngeal nerve more frequently presents a pre-vascular course than the left recurrent laryngeal nerve, as it arises higher than the left nerve and has a more oblique course. In few cases, there is a connecting branch between the inferior laryngeal nerve, a branch of the RLN, and the internal laryngeal nerve, a branch of the superior laryngeal nerve. This is called as anastomosis of Galen.[12]
The course of the nerve should be bluntly dissected using the Reinhoff or a right angle clamp. But extensive dissection of the nerve can increase the risk of neurapraxia or injury to the nerve. Redo thyroid surgery can be performed safely if it is based on (i) complete anatomical knowledge including primary variations and secondary distortion due to initial operation, (ii) surgical experience and skillful technique, (iii) awareness of anatomical disturbances after primary surgery, (iv) support of ancillary electrophysiological technology.
Intraoperative neuro-monitoring (IONM) helps in preventing recurrent laryngeal nerve injury during revision and malignant thyroid surgeries. It is helpful as an adjunct to determine the anatomical landmarks which are obscure. There is no statistical difference in reducing surgical time using IONM.[13], [14]
Conclusion
Routine exposure and good dissection of recurrent laryngeal nerve should be a standard procedure during all thyroid operations. Accurate knowledge of the surgical anatomy of the RLN and its abnormalities, variations and relationships to other tissues is crucial for a safe thyroidectomy, because unexpected anatomical variations of the nerve through its cervical course may cause injury.
Informed Consent
Written informed consent was obtained from patient who participated in this case.
Financial Disclosure
The authors declared that this study has received no financial support.
Conflict of Interest
No conflict of interest was declared by the authors.
References
- J P. Jeannon, A. A. Orabi, G. A. Bruch, H. A. Abdalsalam, R. Simo. Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: a systematic review. Int J Clin Pract 2009. [Google Scholar]
- G R Jatzko, P H Lisborg, M G Muller, V M Wette. Recurrent nerve palsy after thyroid operations-principal nerve identification and a literature review. Surg 1994. [Google Scholar]
- M Hermann, G Alk, R Roka, K Glaser, M Freissmuth. Laryngeal recurrent nerve injury in surgery for benign thyroid diseases: effect of nerve dissection and impact of individual surgeon on more than 27,000 nerves at risk. Ann Surg 2002. [Google Scholar]
- Marcin Barczyński, Aleksander Konturek, Krzysztof Pragacz, Aleksandra Papier, Małgorzata Stopa, Wojciech Nowak. Intraoperative Nerve Monitoring Can Reduce Prevalence of Recurrent Laryngeal Nerve Injury in Thyroid Reoperations: Results of a Retrospective Cohort Study. World J Surg 2014. [Google Scholar]
- Nathan James Hayward, Simon Grodski, Meei Yeung, William R. Johnson, Jonathan Serpell. Recurrent laryngeal nerve injury in thyroid surgery: a review. ANZ J Surg 2013. [Google Scholar]
- F Procacciante, G Diamantini, F Caciolo, V. AbilaliajVisual identification of the recurrent laryngeal nerve during thyroidectomy. Ann Ital Chir 2011. [Google Scholar]
- Marcin Barczyński, Aleksander Konturek, Krzysztof Pragacz, Aleksandra Papier, Małgorzata Stopa, Wojciech Nowak. Intraoperative Nerve Monitoring Can Reduce Prevalence of Recurrent Laryngeal Nerve Injury in Thyroid Reoperations: Results of a Retrospective Cohort Study. World J Surg 2014. [Google Scholar]
- Elham Asgharpour, Eva Maranillo, Jose Sañudo, Aran Pascual-Font, Marc Rodriguez-Niedenführ, Francisco J. Valderrama. Recurrent laryngeal nerve landmarks revisited. Head Neck 2012. [Google Scholar]
- C Page, P Monet, J Peltier, B Bonnaire, V Strunski. Non-recurrent laryngeal nerve related to thyroid surgery: report of three cases. J Laryngol Otol 2008. [Google Scholar]
- T Shao, W Qiu, W Yang. Anatomical variations of the recurrent laryngeal nerve in Chinese patients: a prospective study of 2,404 patients. Sci Rep 2016. [Google Scholar]
- B M Henry, J Vikse, J M Graves, S Sanna, B Sanna, I M Tomaszewska. Extralaryngeal branching of the recurrent laryngeal nerve: a Meta analysis of 28,387 nerves. Langenbecks Arch Surg 2016. [Google Scholar]
- F H Lahey. Routine dissection and demonstration recurrent laryngeal nerve in subtotal thyroidectomy. Surg Gynecol Obstet 1938. [Google Scholar]
- P Angelos. Recurrent laryngeal nerve monitoring: state of the art, ethical and legal issues. Surg Clin North Am 2009. [Google Scholar]
- H Dralle, C Sekulla, J Haerting. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surg 2004. [Google Scholar]
How to Cite This Article
Vancouver
Ray CS, Sahoo KA. Duplication of recurrent laryngeal nerve in thyroid surgery – a rare anatomical variation [Internet]. J Oral Med Oral Surg Oral Pathol Oral Radiol. 2025 [cited 2025 Sep 04];6(2):85-88. Available from: https://doi.org/10.18231/j.jooo.2020.020
APA
Ray, C. S., Sahoo, K. A. (2025). Duplication of recurrent laryngeal nerve in thyroid surgery – a rare anatomical variation. J Oral Med Oral Surg Oral Pathol Oral Radiol, 6(2), 85-88. https://doi.org/10.18231/j.jooo.2020.020
MLA
Ray, Chinmaya Sundar, Sahoo, Krishna Arpita. "Duplication of recurrent laryngeal nerve in thyroid surgery – a rare anatomical variation." J Oral Med Oral Surg Oral Pathol Oral Radiol, vol. 6, no. 2, 2025, pp. 85-88. https://doi.org/10.18231/j.jooo.2020.020
Chicago
Ray, C. S., Sahoo, K. A.. "Duplication of recurrent laryngeal nerve in thyroid surgery – a rare anatomical variation." J Oral Med Oral Surg Oral Pathol Oral Radiol 6, no. 2 (2025): 85-88. https://doi.org/10.18231/j.jooo.2020.020
