- Visibility 58 Views
- Downloads 4 Downloads
- DOI 10.18231/j.jooo.2020.021
-
CrossMark
- Citation
Frontal bone fracture- open reduction and internal fixation with help of titanium mesh
- Author Details:
-
Shandilya Ramanojam
-
Mayur Limbhore *
-
Pallavi Rathi
-
Vikrant Sane
-
Vikram Singh
Introduction
Frontal bone fracture are most commonly fracture due to the projection in the facial region. It accounts for 5-15%[1] of all facial fractures. Depending upon the fracture type, age of patient, medical conditions and aesthetic and functional status the treatment plan should be decided. Before proceeding to the treatment proper evaluation of the patient should be carried out such as GCS status, CSF leak, ophthalmology and neurosurgeon consultations. Most common complication such as meningitis, mucocele and cerebral abscess should be taken into consideration. Etiology consist of RTA, physical assult and sport injury.[2]
Case Report
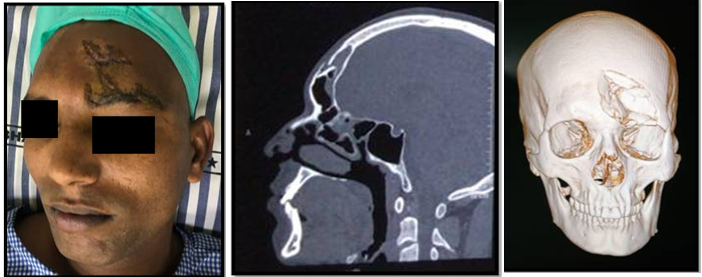
24 years male reported to Bharati hospital Pune with chief complaint of road traffic accident. On examination it was noted that he had contused lacerated wound (CLW) on left side of frontal bone region measuring about 3*3*4cm in diameter. Primary care such as suturing of CLW was done in casualty with help of 3’0 silk sutures. 3D CT scan was advised which revealed fracture of anterior table fracture of frontal bone on left side ([Figure 1]).
Surgical procedure
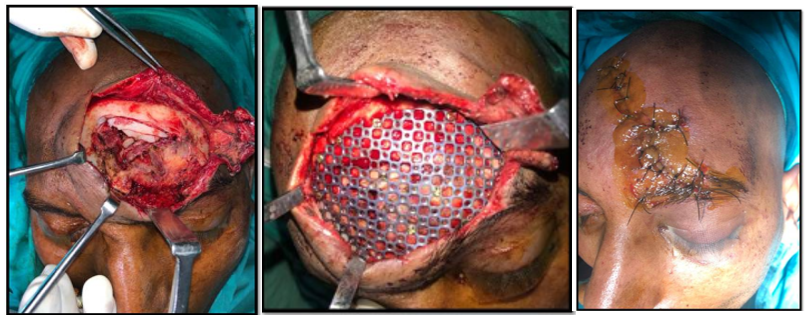
General anesthesia was induced. Oral intubation was done. Painting and draping of operating field was done, 2% lignocaine with 1:200000 adrenaline was infiltrated in the area to achieve vasoconstriction. The fracture site was exposed via extending the existing lacerated wound. It was a depressed comminuted fracture of anterior table fracture of frontal bone. Since it was only aesthetic deformity, the defect was flushed with periosteum intact. Titanium mesh was adapted and fixed at all corners with help of 2*4mm screw. Now a drill was introduced in centre of depressed part of bone and with help of 2*10mm screw, only 2 threads was introduced into the depressed bone and depressed bone was lifted up. Once the bone was lifted the depressed bony fragment was fixed with help of 2*4mm screw and adapted to titanium mesh. This technique help to aligned depressed bone fragment in appropriate position. Through irrigation was done with help of betadine and saline and closure was achieved with 3’0 silk suture ([Figure 2]). Patient recovered from anesthesia uneventfully. He received post operative analgesic and antibiotics for five days. The wound was healed uneventfully. Suture removal was done on seventh day postoperatively ([Figure 3]). Patient was satisfied with the result and no postoperative complications occurred. Patient was followed up for 6 month.

Discussion
Many algorithms for management of frontal sinus fractures vary widely. Appropriate treatment depends on an accurate diagnosis, clinical examination and CT scans. It is not uncommon for post craniofacial trauma patient to require augmentation of depressed craniofacial skeleton. Reconstruction and recontouring of these defects in natural esthetic fashion can pose challenge to clinician.
Various autogenous bone graft and alloplastic materials have been in use for this purpose i.e. titanium mesh, polymethyl methacrylate[3], [4] autogenous bone and hydroxyapatite have been used with varying success. All materials and grafts have merits and demerits in their use.
Titanium mesh[2] is easily available, no secondary site morbidity, ease of use, minimum complications and excellent post-operative results. Infection and foreign body reaction and are few demerits of alloplastic material.
Autogenous bone grafts[5] such as iliac or rib require a second surgical site. This may lead to donor site morbidity, inability to obtain adequate bone for large defect.
Other alloplastic materials[5] that have been used for such defects are hydroxyapatite, silicon rubber, acrylic metal plates and proplast. Growth limitation may be obviated by not placing alloplastic material across sutures in children with enlarging skulls.[6]
Conclusion
Proper diagnosis and treatment plan helps the surgeon to achieve best result. Knowledge about anatomy helps us to achieve proper form and function. Adequate evaluation of the patient help to minimize complications rate.
Source of Funding
None.
Conflict of Interest
None.
References
- Arthur A Gonty, Robert D Marciani, Dominick C Adornato. Management of frontal sinus fractures: A review of 33 cases. J Oral Maxillofac Surg 1999. [Google Scholar]
- E A Luce. Frontal sinus fracture: guidelines to management. Plast Reconstr Surg 1987. [Google Scholar]
- John A. Persing, Arthur J. Cronin, Johnny B. Delashaw, Milton T. Edgerton, Scott L. Henson, John A. Jane. Late surgical treatment of unilateral coronal synostosis using methyl methacrylate. J Neurosurg 1987. [Google Scholar]
- Serge Marbacher, Robert H. Andres, Ali-Reza Fathi, Javier Fandino. Primary Reconstruction of Open Depressed Skull Fractures With Titanium Mesh. J Craniofac Surg 2008. [Google Scholar]
- J B Roberson, W S Rosenberg. Traumatic cranial defects reconstructed with the HTR-PMI cranioplastic implant . J Craniomaxillofac Trauma 1997. [Google Scholar]
- R C Schultz. Restoration of frontal contour with methyl methacrylate. Ann Plast Surg 1979. [Google Scholar]
