Introduction
Oral cancer accounts for the eleventh most typical cancer worldwide.1 Oral squamous cell carcinoma (OSCC) is the most common oral cancer with diverse clinical presentations. It accounts for more than 90% of all malignant lesions in the oral cavity.2 The affected population cluster was <40 years of age in high-incidence countries such as Asian nations like India, Pakistan, and Sri Lanka.3 Alveolar ridge SSC accounts for 9% of all cases with oral SCC.4 Alveolar ridge SSC accounts for the second position, with the primary being carcinoma of the tongue as per site specificity. As per local recurrence rate by site, mandibular alveolus carcinoma has the highest local recurrence rate (26/42), second being carcinoma of the tongue (20/47). Squamous cell carcinomas can occur in all areas of the body, but they are most common in the skin and oral cavity.
OSCC of the mandibular region is found posses an all time low survival rate in comprising with all other oral carcinomas.5 Varied aids used for assessing mandibular invasion include clinical examination, radiographic examination (OPG, CT dentascan, MRI, bone scans, ultrasound, and PET CT), and Histopathological examination. Histopathologic analysis of squamous cell carcinoma reveals two basic patterns of tumor invasion: invasive pattern (infiltrative pattern) and erosive pattern (compressive patterns). Wthin the invasive pattern, islands of tumor infiltrate cancellous spaces with very little osteoclastic activity and no intervening connective tissue. However within the erosive pattern, the tumor advances as a broad front with active osteoclasts separating the tumor from the bone and the connective tissue layer separating the tumor/bone.6
The clinical presentation of OSCC varies from a white plaque to an ulcerated lesion.7 Malignant lesions within the gingiva may resemble oftenly seen inflammatory lesions of the gingiva. Oral carcinomas can usually be misdiagnosed as other inflammatory lesions in the oral cavity leading to delay of treatment. Thus, the early diagnosis and treatment of oral carcinoma by health care providers is mandatory for optimum treatment outcome.8 Most common treatment of OSCC is mainly a surgical excision and a radical neck dissection in the case of lymph node metastasis. Radiotherapy is considered as adjunct postoperative treatment along with chemotherapy and is a definite treatment of choice in case of advanced stages of carcinoma. Oral carcinoma has emerged as a major health problem in India mainly because of the high prevalence of smokeless tobacco use. Oral SCC metastases to regional lymph nodes in the neck and distant metastases are seen in the later stages as diseases progress.9 Here, we are reporting a tobacco-related case of SCC of the lower alveolus with atypical presentation of desquamative gingival lesions and often more chance to misdiagnose the case.
Case Report
A thirty eight year old male patient came to the department of oral and maxillofacial pathology and microbiology with a chief complaint of pain and swelling in the left lower back region of jaw since 2 months.
The patient gave a history of antibiotic and analgesic medication for one week after consulting with a close by hospital. Pain was throbbing type and continuous in nature, and it aggravates on opening the mouth, during mastication, and while brushing teeth.
General clinical examination revealed restricted mouth opening (30mm). Multiple tender lymph nodes were noted on the left side of the face and neck region. On palpation, submandibular and cervical lymph nodes were tender and palpable (2 cm in diameter) and were firm and fixed to the skin. A diffuse swelling was seen on the left side of the face 2.8 cm superio inferiorl 3.4 cm anterio posteriorly. Extending superiorly from ala tragus line Anteriorly upto corner of mouth. Posteriorly upto line joining the outer canthus to the lower border of mandible.
Personal History
Patient had history of tobacco chewing 3-4 packets/day since 10yrs and smoking 2-3 cigarettes /day since 15 years.
The intraoral examination revealed an Ulcero-proliferative growth on left buccal mucosa, involving the buccal vestibule and extending from (35 to 37) premolar to retromolar region.
It was irregular in shape and size, whitish red in colour. Margins were everted and was covered by pseudo- membranous slough.
On palpation, the growth was tender and firm in consistency. The growth was fixed in relation with deeper structures. Periodontal probing resulted in profuse bleeding in relation to 35 to 37 regions. Deep pockets (>6 mm) in relation to the 34, 35, 36 and 37 regions.
Hard tissue examination revealed an end-on-end occlusion. A comprehensive periodontal examination was done and revealed heavy accumulation of calculus on the lingual surface of mandibular posteriors. Generalized cervical abrasion and attrition were present. The oral hygiene maintenance was compromised due restricted mouth opening, severe pain while brushing interfering with proper plaque removal.
Figure 1
38 old male patient complaining of pain and swelling in left lower back region since 2 months

Figure 3
An Ulcero-proliferative growth on left buccal mucosa, involving the buccal vestibule and extending from premolar to retromolar region.

Radiographic evaluation
OPG revealed generalized horizontal bone loss
Based on clinical and radiographic examination, aprovisional diagnosis Chronic Non Healing Ulcer, Oral Squamous Cell Carcinoma was made
Differential diagnosis is Tuberculous ulcer, Fungal granulomatous disease and Verrucous carcinoma.
On gross examination
A small soft tissue bit from incisional biopsy, creamish-brown in color, soft in consistency, ovoid in shape, measuring about 0.8 x 0.6x 0.5 cm in size.
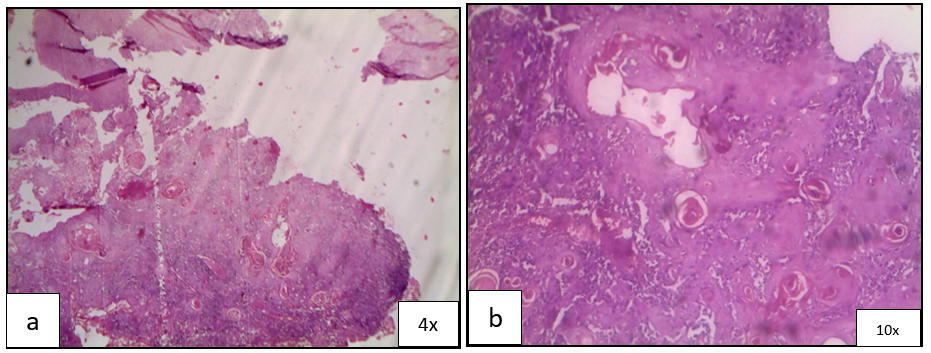
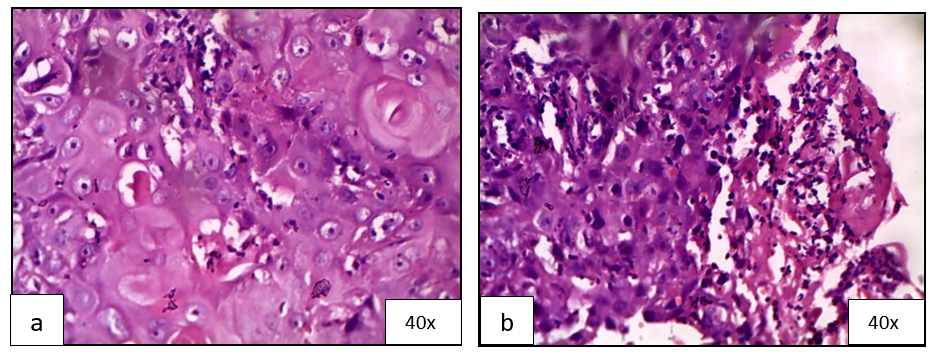
Histopathological examination
The given soft tissue section revealed islands and sheets of malignant squamous epithelial cells breaching into the connective tissue stroma (Figure 7 (a) (b)). The neoplastic cells exhibit numerous keratin pearl formation, nuclear and cellular pleomorphism, and mitotic figures (Figure 8 a,b 40x) seen. Based on clinical, radiographic, and Histopathological examinations, the case is diagnosed as well differentiated squamous cell carcinoma (SCC). The patient was referred to the Regional Cancer Centre (RCC), Delhi cancer institute, for further treatments.
Discussion
Oral squamous cell carcinoma is considered as the most common malignant neoplasm of the oral cavity. The tongue, oropharynx, and floor of the mouth are the most common sites, and OSCC of the gingiva and lips is rarely seen. OSCC of the mandibular gingiva is more commonly seen than the maxillary gingiva.10 Oral carcinomas are mostly associated with tobacco chewing habit and commonly appear as a premalignant lesion giving an appearance of leukoplakia before progressing to the malignant stage, but rare cases have also been reported with nontobacco-associated squamous cell carcinoma. The case reported here is one with the history of tobacco chewing, smoking habit. Carcinoma of the gingival region often resembles desquamative gingival lesions and other inflammatory gingival lesions. In the absence of detailed clinical examination and radiographic investigation there are higher chances of misdiagnosis. The second most common site for oral carcinoma is mandibular alveolus. OSCC is more frequently seen in men compared to women. Its has been reported that men are highly exposed to habits such as smoking and tobacco chewing.
Age is another important factor for oral SCC; as age advances, pronounced genetic and epigenetic changes take place. The case presented here is a male patient of age 38 years with a lesion mimicking desquamative lesion in relation to the left mandibular posterior region. Another important feature of squamous cell carcinoma is regional lymph node metastasis. In case of lower alveolus cervical lymph nodes of the submandibular triangle and upper jugular regions have stronger predilection of regional lymph node metastasis OSCC.11 Tender and palpable submandibular and cervical lymph nodes (which are firm and fixed to the skin) of about 2 cm in diameter were detected in the present case. Prognosis is better in early oral OSCC, especially those that are well-differentiated and without metastasis, the present case was well differentiated OSCC but the worst part is that most cases of OSCC are not diagnosed at the earlier stage of the disease. Based on a number of factors prognosis can vary that are related to the tumor or treatment or to the patient. OSCC was found to enter the medullary cavity through the upper border of the mandible, either only through occlusal ridge or in combination with penetration of either the buccal or lingual plates. Another important route of entry the spread through the foramina. When the carcinoma is not that deep, that is, if it does not reach the alveolar canal, then there is no spread along the alveolar canal and little or no insinuation of the cancer cells beyond the tumor front.12 The radiologically investigated bone defects in squamous cell carcinoma were classified as follows: (a) Erosive type having well defined margins of the absorbed bone and (b) moth eaten—irregular type, ill-defined margins of absorbed bone. Histopathologic patterns of bone involvement were classified as follows: (a) expansive type the outline of the eroded bone appears smooth or slightly concave and (b) infiltrative type: tumors will infiltrate the mandible through spaces or aggressively by destroying the bone. The extent of radiologically detected bone defects and the histological pattern of bone involvement can be graded as follows: (a) grade 1: bone defects limited to the alveolar bone, (b) grade 2: bone defects exceeded the alveolar bone but did not extent beyond the mandibular canal or the temporary line between right and left mental foramen, and (c) grade 3: bone defects extend beyond the mandibular canal or the temporary line between the right and the left mental foramen.13 The case presented here shows generalised horizontal bone loss.
A surgical excision followed by radiation therapy and chemotherapy as postoperative adjunct treatment modalities is primary treatment of squamous cell carcinoma. In case of lymph node metastasis radical neck dissection is often required. When the bone defects did not extend beyond the mandibular canal Marginal resection is considered as a treatment option and segmental resection if it extends beyond the mandibular canal. About 78.1% is the 5-year cumulative survival rate for the mandibular marginal resection group and 72.8% in the segmental resection group.13 Other innovations in the field of cancer therapy were laser based technology (photodynamic therapy), immunotherapy, and gene therapy to treat oral squamous cell carcinoma at very earlier stage.14 The case present here was also on photodynamic therapy in Delhi cancer institute GTB.
Conclusion
Oral Squamous cell carcinoma is the most common malignant epithelial neoplasm with varied oral presentations. Therefore, the dentist/oral pathologist should be aware of the characteristics of the disease. As the disease progresses the most fatal complication is the distant metastasis. Thus, correct and timely diagnosis is of utmost importance and there are more chances for misdiagnosis as the clinical presentation of oral squamous cell carcinoma can resemble inflammatory gingival lesions.