- Visibility 99 Views
- Downloads 11 Downloads
- DOI 10.18231/j.jooo.2020.035
-
CrossMark
- Citation
Epidermoid cyst: A menace to facial cosmesis – Case report
- Author Details:
-
Rajesh Kshirsagar
-
Pratik Warade *
-
Prasamita Mishra
-
Vikram Singh
-
Pranave P
Introduction
An epidermal cyst is derived from the epidermis, and is formed by cystic envelope of epithelium within the dermis that becomes filled with keratin and lipid-rich material or debris. Epidermoid cysts are slow-growing benign subcutaneous lesions imposing as nodules or tumors. Only about 7% are found in the head and neck region.[1] Giant epidermoid cysts > 5 cm in diameter can cause problems, especially in the head-and-neck region and sole.[2] As facial esthetics is of prime concern in modern day routine, the appropriate treatment modality will help an individual to regain back his/her confidence in society.
The most affected area in the head neck region is floor of the mouth, along with the tongue, lips, buccal mucosa and mandibular bone.[3], [4]
For the ideal treatment modality it is necessary to diagnose the lesion accurately. Because of its variable clinical presentation it is advisable to use specialized or advance imaging techniques such as CT (computed tomography) or MRI (magnetic resonance imaging). Histopathological examination is the gold standard where you will get stratified squamous epithelium with a granular layer which contains keratin.
We describe a case of patient having an large growth in left mandibular region suggestive of epidermoid cyst and will be discussing its features such as age of onset, anatomic location, differential diagnosis, diagnostic findings and the treatment done for the same.
Case Report
A 30 year old male reported to the department of oral and maxillofacial surgery with a complaint of swelling on left side of lower jaw ([Figure 1]). The swelling was present since 10 years. Initially it was small in size, non tender and progressed to present size. On examination the swelling was oval in shape, asymptomatic and insidious in onset measuring about 6.2 x 4.9 x 6.6 cms. There was no history of trauma or any discharge.
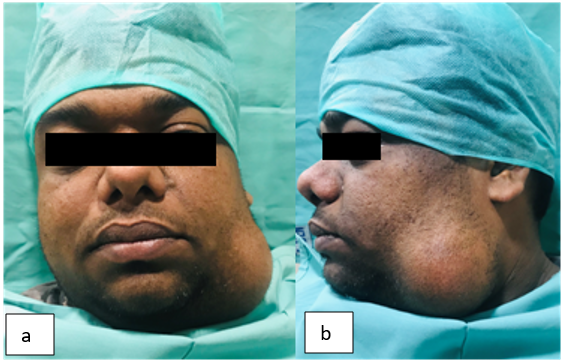
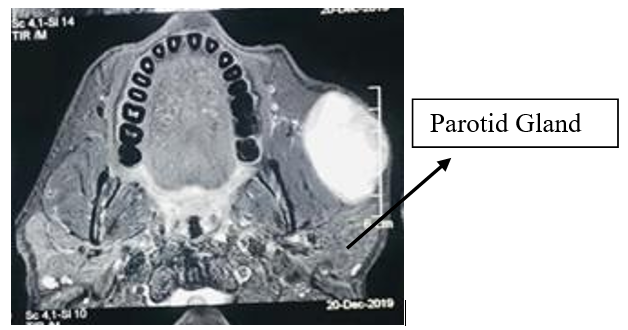
On palpation, the swelling was afebrile, soft, non-tender, fluctuant and non adherent to the underlying skin. Color of the swelling was same as of the underlying skin. Advanced diagnostic imaging includes head and neck MRI with contrast and CT suggestive of large well defined peripherally enhancing lesion within the subcutaneous soft tissues anterior to the left parotid gland with mass effect on the adjacent muscles indicative of an epidermal inclusion cyst ([Figure 2]).
Due to previous unfavorable experiences patient was reluctant to undergo any procedure under Local anaesthesia and was keen on getting the aesthetic correction done. Patient also denied for FNAC. Therefore complete excision of the lesion under General anaesthesia was the treatment plan decided post patient’s counseling regarding all possible risks and complictions. Following all aseptic conditions and precautions Local anaesthesia (1:200000) was infiltrated. Elliptical devolving incision was marked over the most dependent part of the swelling ([Figure 3] a). Following the surgical exploration the mass has been removed uneventfully ([Figure 3] b & c). The extra tissue has been excised and closure done with subcutaneous suturing to avoid possible scarring and a drain was placed ([Figure 3] d). The histopathological examination confirmed the diagnosis of epidermoid cyst. ([Figure 4])



Discussion
Histologically and in accordance with the classification described by Meyer in 1955 term dermoid is a distinct entity that is normally used to indicate three different types of cyst: the real dermoid (comprises skin appendeges), the epidermoid (enclosed in epithelium) and the teratoma (includes muscles, cartilage and bones). In a 20-year study, it has been seen that dermoid and epidermoid cysts consist of only 3.7% of all congenital non-salivary cysts of the suprahyoid neck in children.[5] Dermoid cysts are generally found in the midline[6] especially in the areas of embryonic fusion, either following sequestration of ectodermal tissue, or due to failure of separation of the ectoderm from the mesoderm during 3rd–5th weeks of gestation.[7] The most common location in the head–neck region is around the eyes, followed by dorsum of the nose and anterior aspect of neck. Epidermoid cysts are slow growing and usually asymptomatic but they become inflamed or secondarily infected resulting in pain and tenderness. The cyst can occur at any age most common in the third and fourth decades of life. Advance imaging such as MRI, CT contrast has an important role in confirming the diagnosis and classifying cysts according to their relation to muscle. Histopathological examination is the gold standard but as in this case due to unfavourable previous experiences of the patient regarding the procedures under local anaesthesia this option was excluded.
Pathological features of epidermoid cysts are oily or cheesy, tan, yellow white material and the cyst wall is a fibrous capsule usually 2-6 mm is thickness.
The term Traumatic Epidermoid cysts and Epidermoid Inclusion Cysts describe the same phenomenon, and both indicate a traumatic etiology. The epithelial implant theory is the most widely accepted. It proposes that epidermal structures are driven into deeper tissues. The trapped epidermal structures assume the role of a skin graft and become independent. The tissue continues growing in its new position and produces keratin, thus forming a cyst. The differential diagnoses of a clinically benign cystic lesion in the head–neck region include an array of developmental and acquired lesions, but those involving the floor of the mouth and neck are less in number, like, thyroglossal duct cyst, ranula, cystic hygroma, cystic lymphangioma, mucocele, branchial cleft cyst, haemangioma and infective lesions.[8]
In this case the chances of cyst originating as a result of entrapment have been ruled out as there was no history of trauma and previous surgical treatment in that area. Therefore surgical excision remains the best treatment modality, which also gave satisfactory esthetic outcomes. On the basis of clinical and histological examination the diagnosis of epidermoid cyst was confirmed.
Conclusion
The entity that is epidermoid cyst is very rare and uncommon in head and neck region. Often it gets misdiagnosed. Facial asymmetries often deteriorate a person’s self confidence. In the era of advanced diagnostics aids it becomes feasible to plan an appropriate treatment and to get back the patients smile. Early diagnosis and complete surgical excision is of utmost paramount.
Source of Funding
None.
Conflict of Interest
None.
References
- T Kandogan, M Koç, E Vardar, E Selek, Ö Sezgin. Sublingual epidermoid cyst: a case report. J Med Case Reports 2007. [Google Scholar]
- S B Ramakrishnaiah, S S Rajput, N S Gopinathan. Epidermoid cyst of the sole - a case report. J Clin Diagn Res 2016. [Google Scholar]
- A B Bataineh, M J Mansour. Extraoral epidermoid cysts. Br J Oral Maxillofac Surg 1997. [Google Scholar]
- T Kandogan, M Koç, E Vardar, E Selek, Ö Sezgin. Sublingual epidermoid cyst: a case report. J Med Case Reports 2007. [Google Scholar]
- Y Y Hsieh, S Hsueh, C Hsueh. Pathological analysis of congenital cervical cysts in children: 20 years of experience at Chang Gung Memorial Hospital. Chang Gung Med J 2003. [Google Scholar]
- J P Dabholkar, A D Patole, A S Sheth, R Saaj. Congenital cystic lesions in head and neck. Indian J Otolaryngol Head Neck Surg 2003. [Google Scholar]
- J Mathews, J Lancaster, G O’Sullivan. True lateral dermoid cyst of the floor of the mouth. J Laryngol Otol 2001. [Google Scholar]
- M F Burger, P Holland, B Napier. Submental Midline Dermoid Cyst in a 25-Year-Old Man. Ear, Nose Throat J 2006. [Google Scholar]
