Introduction
Metastatic tumors are the commonest malignant neoplasm of the skeleton in general.1 For the diagnosis of the malignant tumors of the oral cavity, it is necessary to take into account the possibility of both the primary as well as the metastatic tumors.2 Metastatic tumors to the jaw are a rare phenomenon, representing about 1–4% of oral malignancies that are metastasis from a distant primary site.3
The most common principal source of metastatic tumors to the oral cavity or maxillofacial area are the breast, lung, prostate, kidney, bone, colon and rectum, thyroid, stomach, testis, bladder, ovary and cervix.4, 5 The breast forms the commonest primary site for tumors that metastasize to the mandible and lung is the preferred site for tumors that metastasize to the oral soft tissues.6 The cervical lymph nodes, mandible and gingiva are the most commonly affected areas by the metastatic tumors.7 In the mandible, molar area is the preferred site for metastatic tumors8 and the gingiva is the commonest site for metastatic colonization in oral soft tissues.9, 10
In this review, we have highlighted the various predisposing factors and propose hypothetical pathways of lung carcinoma metastasizing to the different areas of the body including the oral cavity.
In considering oral tumors, only 1–3% of oral malignancies are metastatic from a distant primary site, in decreasing order, from the breast, adrenal gland, colorectal system, genital organs and thyroid gland in females and from lung, prostate, bone and adrenal gland in males.7, 11
Lung cancer is the most commonly diagnosed major cancer in the world that mainly arises from the epithelial cells. The lung is the most preferred site for the metastasis of tumors from other parts of the body. The 2 most common forms of lung cancer are Non small cell and Small cell lung carcinoma12 and the major cause is from the carcinogenic effect of cigarette smoke, making it the leading cause of cancer death worldwide.12, 13 The major symptoms of lung cancer are cough, hemoptysis, weight loss and shortness of breath.13
Predisposing factors (Figure 1) that may play a role in lung cancer are tobacco smoke accounting for 80 - 90% of cases12, 13 and Non - smokers accounting for the remaining 10 -15% of lung cancer.14 The other factors are industrial hazards such as uranium and asbestos,13 radon gas,13, 15, 16 genetic alterations that includes activation of oncogenes such as C- MYC, K – Ras, EGFR and Her 2/ neu17, 18 and inactivation of tumor suppressor genes such as p53, RB, p 16 INK 4a 19, 20 and air pollution.13 About 4% of Non-Small Cell lung carcinoma involves EML4 – ALK tyrosine kinase fusion gene and Small Cell lung carcinoma may be derived from neuro -endocrine cells, club cells, and neuro – epithelial cells and these cancers may express CD 44.17
The cancer that originates in the lung are called primary lung carcinoma and the most common site of metastasis of primary lung cancer are bone, brain, liver and supra – renal glands. Secondary cancers that spread to the lungs are breast, colon, and prostate and bladder cancer.
Metastasis of Lung cancer (Figure 2) occurs by 3 routes namely direct, hematogenous and lymphatogenous spread. In the direct spread of lung cancer, involvement of the phrenic nerve results in paralysis of half of the diaphragm. Apical lung cancers are associated with recurrent laryngeal nerve (branch of vagus nerve) because of its close proximity to the apex of the lung.
Carcinoma arising from the right lung spreads to the heart, inferior and superior vena cava, azygous vein and esophagus and those arising from the left lung spread to the heart, aortic arch, thoracic aorta and esophagus. 21
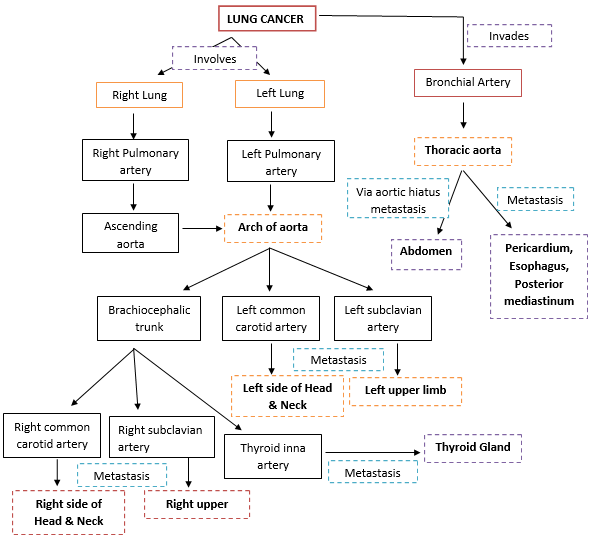
Overview of hematogenous spread of lung cancer is outlined in Figure 3.
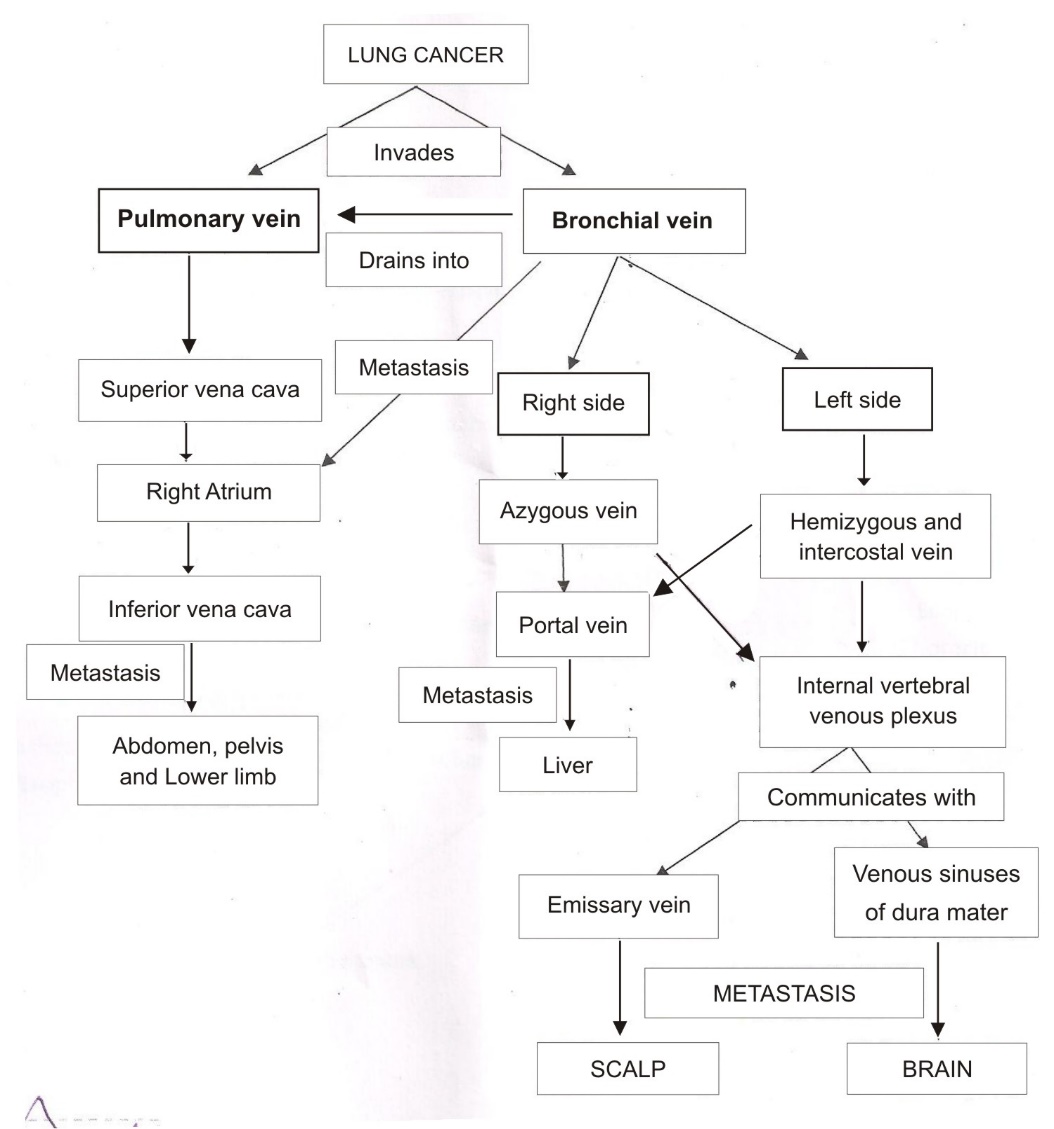
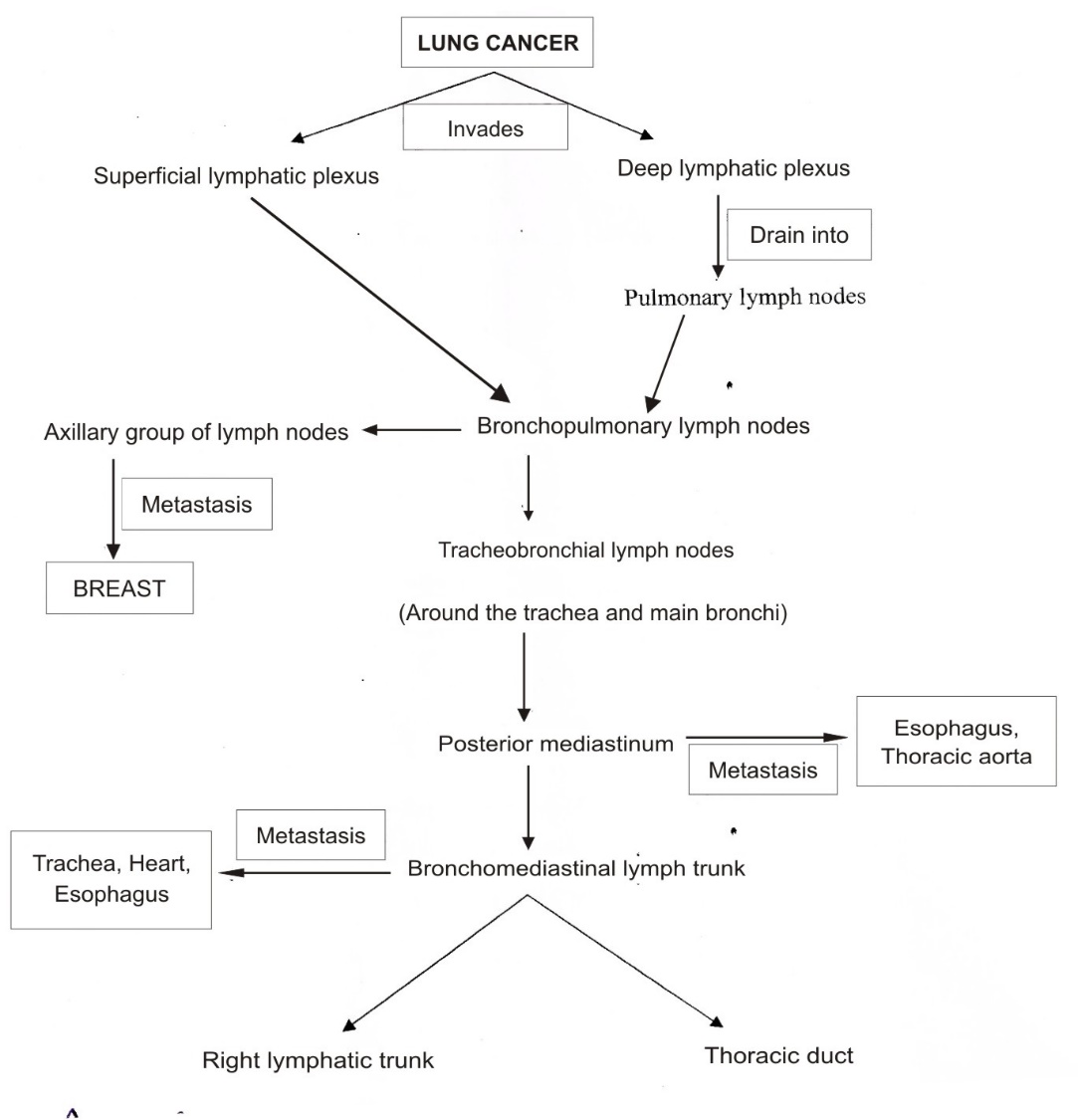
The tumor cells enter the systemic circulation by invading the wall of vessel of the lung which is then transported via the pulmonary veins, left heart and aorta. This constitutes the venous drainage (Figure 4) which forms another route for the metastasis of lung cancer. The route of metastasis of lung cancer occurs via lymphatic spread is outlined in Figure 5.
This lymph thus carries the cancer cells into the venous system and right atrium of heart. The cancer cells after passing through the pulmonary circulation are carried back into the heart, from where they are distributed to the entire body.
Lung cancer is mostly detected on the chest radiographs and CT scans can also be used as a diagnostic modality to detect lung cancer. These lung cancers are confirmed by biopsy, which is usually performed by either bronchoscopy or under CT – guidance. The various treatment modalities that can be used for these lung carcinomas include surgery, chemotherapy and radiotherapy.
Conclusion
Oral cavity has been described as a reflection or mirror of systemic diseases. Oral manifestations are often the sole indication of the disease and also the first indicator for the presence of malignant tumors. With the advent of Immuno – histochemical markers and advancement in molecular techniques, the diagnosis becomes easier and a better understanding of the biology of the tumors can be achieved, so that the newer therapies targeting the molecular level may be introduced to halt the tumor proliferation, thereby improving the quality of life as well as life expectancy of the patients.