Introduction
The angle of the mandible can be defined as the junction between the body of the mandible and the ramus at the origin of external oblique line.1 Fracture in this region usually results from fall, road traffic accidents, interpersonal violence or as a complication of mandibular 3rd molar extraction.1 About 25-35% of all the fractures of the mandible are in the mandibular angle region.2 The fracture line can be horizontal/vertical. It can be further classified as favorable (undisplaced) and unfavorable (displaced).3 Treatment of this fracture has evolved from old bandaging and splinting methods to the latest 3-Dimensional (3D) reconstruction plate with varying success levels.4 Yet no single treatment modality is considered ideal for the treatment of angle fracture. The concept of angle fracture management took a complete transformation with evolution of Champy’s “Modified Michelet Technique”, wherein he advocated the placement of a single plate along the external oblique ridge vertically as per his line of osteosynthesis.5 The results of such a platting was very desirable,6 but an increase in the rate of post-operative infection was observed. This may be attributed to fact that the incision line lies over the plate and also there will be a 3-Dimensional change that occurs in the plate while adapting it to the external oblique ridge, which may reduce its rigidity and cause movement of fracture segments post-operatively leading to the chain of post-op complications. On the contrary the lateral cortex of the mandible may be plated via a trans-buccal approach. The plate is adapted to the flat surface of the mandible on the lateral aspect. As the incision line won’t lie on the miniplate and the plate is adapted over a flat surface there is no 3-Dimensional changes that occur in the plate, thereby reducing the rate of post-op infection and wound dehiscence.7, 8, 9 Very few studies have been made regarding the outcome and complications of these two techniques. Hence this study aimed to compare the post-operative outcomes of these two techniques for the mandibular angle fracture management.
Materials and Methods
A retrospective study was conducted of the inpatient medical records of patients treated in a specific protocol described below for the mandibular angle fractures at the department of Facio-Maxillary Surgery, Sanjay Gandhi Institute of Trauma and Orthopaedics. The inclusion criteria were: patients with angle fracture that required open reduction and internal fixation, aged between 18-60 years irrespective of gender. Based on the age, patients were classified as younger aged -18 to 30 years, middle-aged 31 to 50 years, and older age - above 50 years. The exclusion criteria was- patients categorised under American association of anaesthesiology class (ASA)III, IV, V, VI, infected fracture site, comminated fractures, patients who were treated by closed reduction, patients with secondary deformity corrections. A total of 40 patients were included in the study. 23 of them were treated by external oblique ridge plating and 17 of them were treated by lateral cortical plating methods. The patients were randomly selected for the external oblique and lateral cortical plate groups. In all patients fractures were reduced with prefabricated upper and lower Eric’s arch bar fixation as a means for intermaxillary fixation intraoperatively. All patients were operated under general anaesthesia, by the same team of surgeons, and the chief operating surgeon with an experience of 15 years, following routine haematological, biochemical, general physical examination and routine radiological examination.
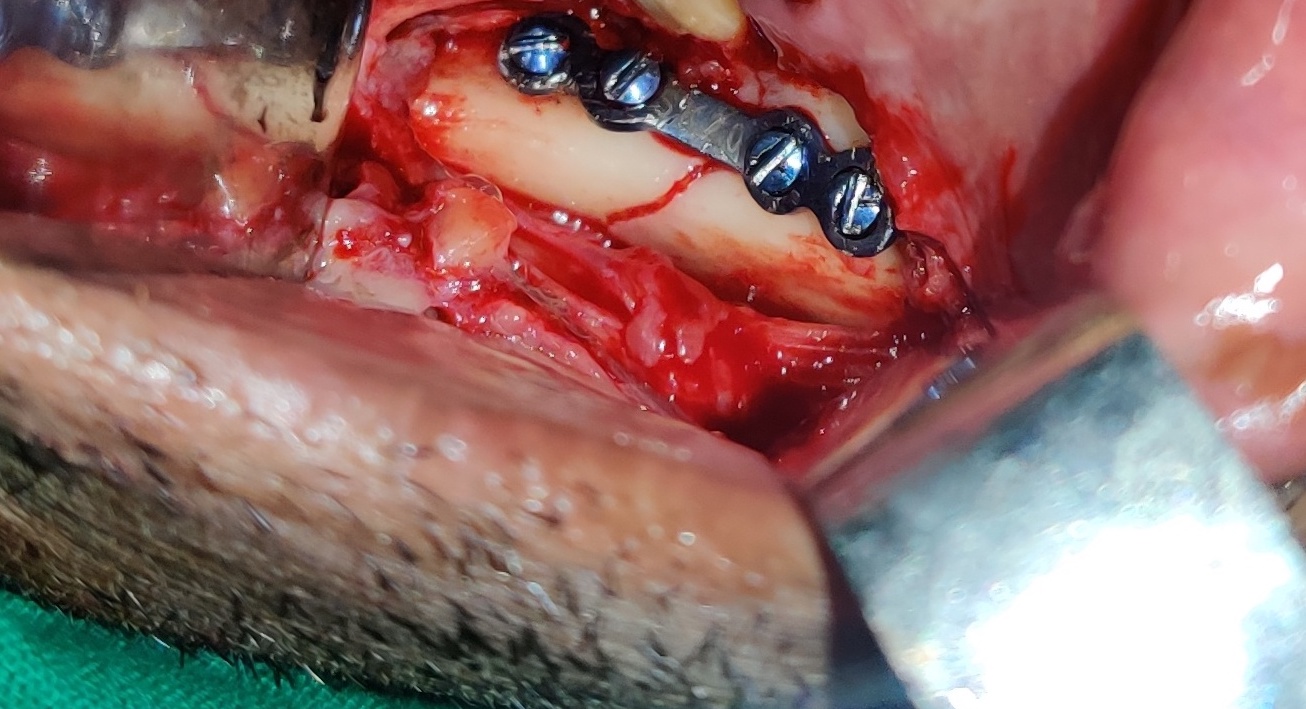
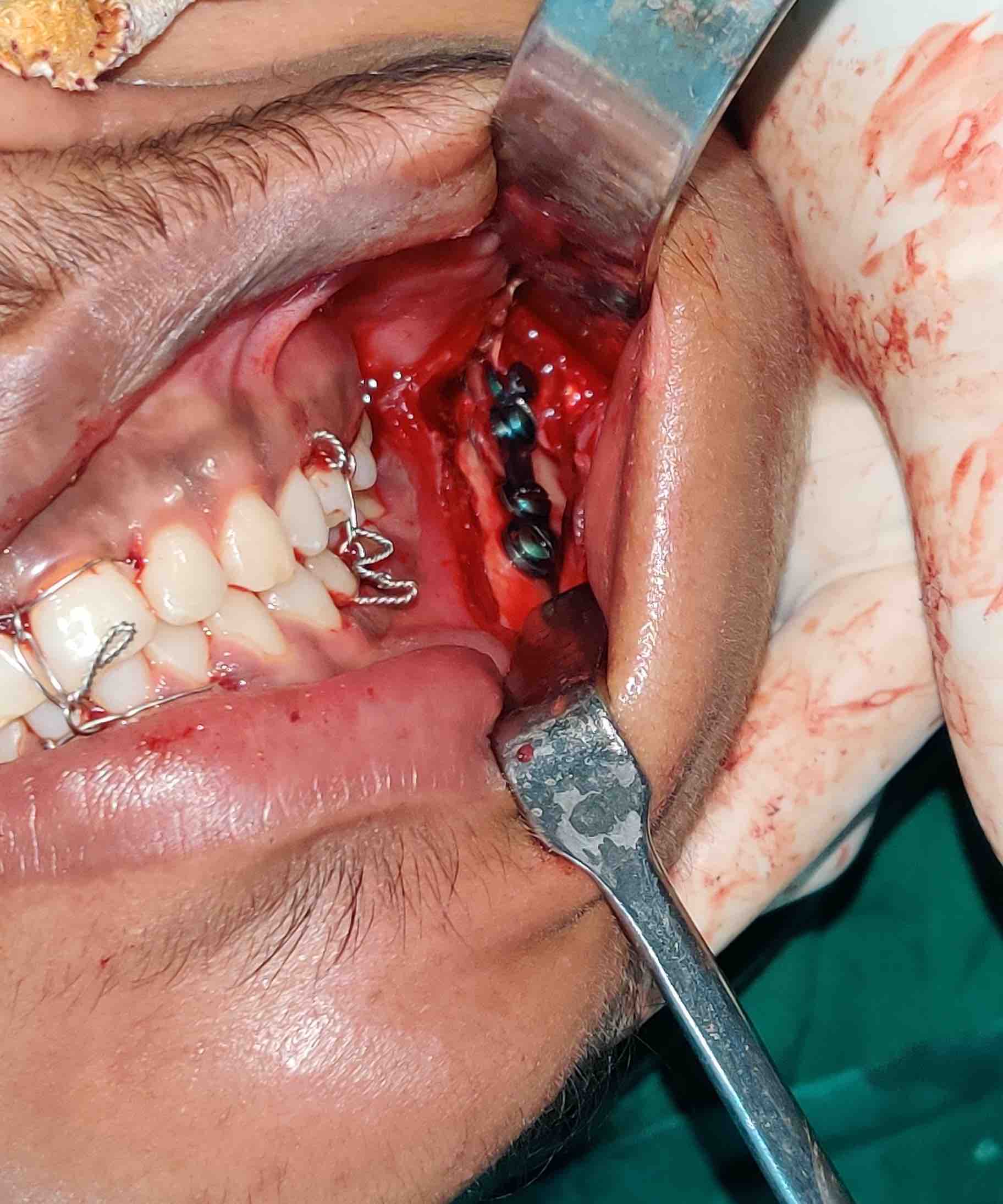
For both the techniques, the retromolar region was infiltrated with local anaesthesia (adverse drug reaction checked priorly). An incision was placed over the anterior border of ascending ramus, extending down anteriorly along the external oblique ridge up to second molar region and the fracture site was exposed. In the external oblique ridge group, the fracture segments were reduced and a single 4-hole with gap titanium miniplate of thickness 2mm was adapted to the external oblique ridge and fixation was done by placing screws 8mm in length, in the sagittal direction (Figure 1, Figure 2, Figure 3, Figure 4Figure 5, Figure 6). For the lateral cortical plating, fracture segments were reduced and a single 4-hole with gap titanium miniplate placed flat to the lateral cortical plate and fixed with screws 6mm in length via a trans buccal approach (Figure 7, Figure 8, Figure 9, Figure 10, Figure 11, Figure 12, Figure 13 ). Completely erupted 3rd molars and which aided in the reduction of the fracture were retained and the 3rd molars which were partially erupted/ unerupted/ infected/ in the line of fracture which compromised the ideal fracture reduction were removed in both the groups. Intra-op and post operative stability of the fracture segments were checked by bi-digital palpation. Water tight closure of the fracture site was done with 3-0 absorbable sutures and were removed by the end of 7-10 days for both the groups. All patients were followed up for a period of 6 months with orthopantomogram taken at the end of 1st, 3rd, and 6th month. All the patients were advised a soft diet for 6 weeks.
Charts of patients were reviewed for age, gender, presence of other fractures, type of plating, operating time(OT) time, which was calculated from the beginning of the incision till the closure, and complications such as post-op infection, wound dehiscence, malocclusion, breakage of plate, mobility of fracture segments, implant retrieval, and non-union.
Results
There were a total of 40 patients with mandibular angle fracture who underwent open reduction and internal fixation. 23(60%) of them were treated with external oblique ridge plating and the remaining 17 (40%) of them with lateral cortical plating. Male patients formed the majority (93.3%) in lateral cortical plate group and 100% in the external oblique ridge plating (p value 0.85). The mean age of the patients in the study group was 32.40 years with a standard deviation of 11.980 (Table 1 ). Main etiology of injury was road traffic accident, in both the groups. 4.3% of the cases in external oblique ridge group and 12.5% in the lateral cortical plate group were bilateral angle fractures with the p value of 0.90. 52% of the external oblique ridge cases and 68.9% of the lateral cortical cases were associated with other fractures. The mean operating room time for external oblique ridge plating approach was 39.78 minutes when compared to 45.47 minutes lateral cortical plating approach. Malocclusion was seen in 10% of external oblique ridge group and none in the lateral cortical plate group with a p value of 0.07. This was due to the presence of associated condyle fractures which were managed by inter-maxillary fixation for a period of 3 weeks. Post of infection and wound dehiscence was observed in 12.5% and 10% of cases respectively in the external oblique plating group and 2.5% and 5% cases respectively in the lateral cortical plating group with the p value of 0.16 and 0.62 respectively (Table 3). This was managed by wound debridement and administration of oral antibiotics and re-suturing of the wound. By the end of 4th post-operative week, mobility of fracture fragments was seen in 2 patients in the external oblique ridge group. This was due to the breakage of the non-compression plate (Table 2). Implant retrieval was performed in these cases and a reconstruction plate was place at the lower border of mandible via extra oral approach. (Table 4). By the end of 8th post-op week non-union was evaluated clinically by the absence of mobility of fracture fragments and confirmed radiologically with orthopantomograph by the end of 12th post-op week.10 No evident unfavorable extra-oral scar was observed post-operatively in any of the lateral cortical approach cases.
Table 1
Distribution of the subjects based on age
|
Age(in years) |
Frequency |
Percent |
|
18 to 30 |
23 |
57.5 |
|
31 to 50 |
11 |
27.5 |
|
50 above |
6 |
15.0 |
|
Total |
40 |
100.0 |
Table 2
Cross-tabulation of type of plating and breakage of plate
Table 3
Cross-tabulation of type of plating and post-op infection
Table 4
Cross-tabulation of type of plating and clinical features
Discussion
Angle fractures are the most problematic in the facial region because of difficult surgical access to the site and high frequency of complication.1, 2, 4 Following rigid internal fixation of these fractures infection and nonunion are commonly reported.5 There is some controversy on the ideal fixation scheme for these structures despite significant results. We intended to compare replacement of non-compression miniplates in two different regions, for the treatment of angle fractures in terms of outcome and complications. In the present study, angle fracture was observed in the age group ranging from 18 to 60 years and the mean age was 32. 40 years. Based on the age, patients were classified as younger aged -18 to 30 years, middle-aged 31 to 50 years, and older age - above 50 years. Out of the 40 patients included in the study, 23 belonged to the younger age group, 11 to the middle age group and 6 to the old age group, indicating that majority of the angle fractures occurred in younger age group, and road traffic accidents being the most common cause of it. This result was consistent with the results of the study conducted by Olikarinen et.al, and Sakr et.al, who reported that a peak incidents of angle fracture was observed between 20-29 years,11, 12 which probably is attributed to the presence of relatively high incidence of un-erupted third molars. Our study consisted of 95% of male patients and 5% of female patients as seen in other studies. This observation was in consistent with that of the study conducted by Dongas et al.,13 who reported male predominance in angle fractures due to the fact that they are more exposed to the risk factors for facial trauma as they get involved in violent conduct, drive recklessly, physical aggression and contact sports. Road traffic accidents was the main etiology (97.5%) when compared to self-fall (2.5%). No assault cases were reported in our study. Ugboko et al., in his study also reported that road traffic accidents were the main cause of angle fractures.14 This could be attributed to multiple reasons such as inadequate road safety awareness, use of alcohol or other intoxicating agents, violation of speed limit, behavioral disorders and socio-cultural insufficiencies. Left side fracture predominance (2.5%) was observed in our study. This was in agreement with the study finding of Inaoka et al. Where they prove that left side had more angle fracture than the right side.15 This did not present any significant relationship with the incidence of angle fracture. The side of impact is usually restricted to the side of fall. If the impact is of a high force or concentrated over a large area than a direct fracture at the point of application, force will transfer to the contralateral side causing and indirect fracture.11 In case of altercations considering the predominance of right-handed people in the society when the victim is facing the opposite direction the site of fracture is related to the side of impact. The rate of complications is slightly high for the external oblique ridge group when compared to the lateral cortical plating group. Post-op infection and wound dehiscence was seen in 12.5% and 10% respectively of the external oblique ridge group when compared to the 2.5% and 5% respectively of the lateral cortical plating group (Table 4). This is in consistent with the study by Ellis and walker, who reported a higher infection rate (25%) and an overall complication rate of 28%.16 Iizuka and Linqvist described an infection rate of 6.6%.17 Fox and Kellman reported a lower rate of local wound infection and dehiscence (2.9%),18 whereas Seemann et al. Described an incidence of 5.9%.19 This could be accounted for the ridge plate being placed superficially on the ridge making it prone to exposure and consequent infection from breakdown of the wound. This was managed by through wound debridement, re-suturing, chlorhexidine mouth rinses and a course of oral antibiotics. Intra-operative time was measured from the beginning of incision till the plate fixation, which was found to be approximately 39.78 minutes for the external oblique ridge group and 45.47min for the lateral cortical plate not much of a difference in both the groups. This is in agreement with the study done by Laverick et al. who observed 320 patients and concluded that mean plating time for fractures were 55 minutes and 60 minutes for the ridge plate and trans buccal plate respectively.20 The 5% breakage of plate that occurred in the external oblique ridge plating group were unfavorable mandibular angle fractures. When a single miniplate is fixed along the external oblique ridge the axial load is shifted from the superior border (tension side) to the inferior border (compression side) leading to poor results in terms of stability, especially in unfavorable fractures. On the contrary the lateral border plate is placed in a more neutral position between the compression and tension zones of the fracture thereby increasing the stability of the fractures especially in unfavorable fractures. 8 There are also the three-dimensional bends that are placed in the ridge plate to contour it to the external oblique ridge which reduces its rigidity. As for the trans-buccal plate, The single miniplate fixed along the external oblique ridge via an intraoral approach, shifts the axial load from tension side to inferior border of mandible leading to poor results in terms of stability and requires IMF for additional stability post operatively. In transbuccal approach the fixation of plate laterally on angle of mandible, allows the plate to be placed in a more neutral position between tension and compression side of fracture and hence hardly requires any bending of plate.
Is placed deeper within the tissues, flat on the mandible with no dimensional changes.20 To epitomize, the ridge plate acts as a tension band with no inferior border control, which is virtually approximated against each other by the compressive force exerted by the muscles attached to the angle region, making the fracture stability debatable. Whereas the lateral cortical plate is adapted over the neutral point, which has control over both the borders and thereby assuring stability of the fracture segments.
Conclusion
To conclude lateral cortical plate fixation is the simplest and better method for the treatment of mandibular angle fractures compared to external oblique ridge fixation as it is a safe and reliable method with minimal complications. Hence this technique is recommended for the fixation of mandibular angle fractures for better stability and for better outcome.