Introduction
Temporomandibular joint is the articulation between squamous part of the temporal bone and head of the condyle of the mandibular. It is a complex joint with unique characteristic and functions. Among the changes in joint hypermobility, dislocation of temporomandibular joint (TMJ) refers when the mandibular condyle is displaced anteriorly beyond the articular eminence, in 1832, Sir Astley cooper introduced the term complete dislocation/luxation and imperfect dislocation/subluxation.1, 2
Three factors contribute to the pathophysiology of mandibular dislocation. (1) Loosening of the capsular and the TMJ ligament (2) prominent eminence (3) Spasm of the muscles of the TMJ.Initially, loosening of the capsule and ligaments allows the condyle to perform excessive motions, through the articular eminence. simple activities such as laughing & yawning, dental consultations, performing intubations, and in episodes of vomiting can results into TMJ dislocations.3 Eminence works as a mechanical barrier & helps to control mandibular motion, this non-functional bypass leads to spasm of the associated muscles of the TMJ. Other aetiological factors which are associated with TMJ dislocation are (1) Trauma (2) The use of drugs such as anti-emetics and phenothiazines which produce extra pyramidal effects on the TMJ (3) Systemic diseases such as rheumatoid arthritis, neurological, Psychogenic, collagen & connective tissue disorder.4 Several imaging techniques are used for evaluation of the TMJ. Among them, MRI has advantages over other techniques depicting soft tissues of TMJ while not relying on ionizing radiation.
Literature contains evidence of both surgical as well as non-surgical treatment modalities.5
Includes
Augmentation of articular eminence
Capsular plication
Temporalis tendon scarification
Condylectomy
Lateral pterygoid myotomy
But these modalities predispose the patient to additional risks of general anaesthesia6
The non-surgical modalities include
The restriction of mandibular movements along with soft diet.
Injection of sclerosing agents into the TMJ. (sclerosing agents which are used in TMJ are hypertonic saline, tetradecyl sulfate, polidocanol, chromated glycerine.
Injection of botulinum toxin into the muscles of mastication.
The application of local anaesthetic into the TMJ.7
In our paper we highlighted the importance of Autologous blood injection in neurologically disordered patient.
Case Report
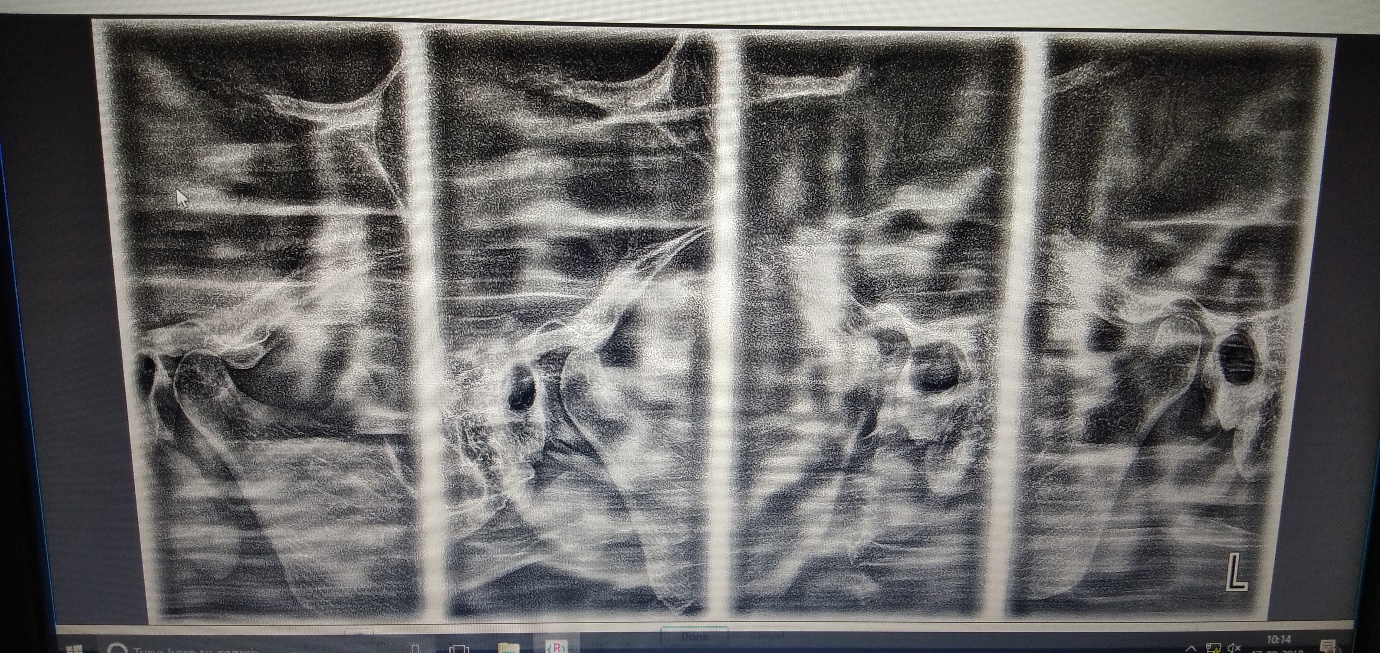
A 45-years-old female reported to Department of Oral and Maxillofacial Surgery Government Dental College & Hospital Mumbai, with chief complaint of recurrent bilateral TMJ dislocation which was dislocated almost 10-12 times in 6 months of duration with a past medical history of neurological disorder (Parkinson’s disease along with dementia) in the last 5 years. On general examination patient was pale, malnourished & disoriented. (Figure 1) On clinical examination mouth opening was reduced, (Figure 2) tenderness to palpation in the pre-auricular region was noted, inability to speak & masticate, mandibular lateral and protrusive movements were normal. Radiologic examination was undertaken with a panoramic radiograph and computed tomography (CT). The panorex showed bilateral anteriorly displaced mandibular condyles well beyond the articular eminences. (Figure 3) The CT confirmed the panoramic findings. The patient and her family were not willing to undergo surgical treatment, due to her neurological disorder & her poor general condition. So, it was decided to treat this chronic recurrent dislocation by autologous blood injection. The procedure was performed under local anaesthesia in an outpatient clinic.
A detail case history, haematological & radiological investigation of the patient was done. The patient was taken into OT after informed consent & parts preparation was done. Infiltration & auriculotemporal nerve block was given in the pre-auricular region. Pre-operative markings were done, a point was then located 10 mm anterior to the tragus and 2 mm inferior to the tragal-canthal line (Figure 4). At this point, a needle (18 Gauge) was inserted into the upper joint space of the temporomandibular joint and the second needle was inserted 20 mm anterior and 10 mm inferior to the tragal-canthal line in the upper joint space. Lavage of the TMJ was done (To remove inflammatory and dead cells in the joint) with approximately 5 ml of Ringer’s lactate solution. Approximately 3 ml of blood was then withdrawn from antecubital fossa of the patient with 20-gauge needle (Figure 5). 2ml of blood was injected into the upper joint space of TMJ and 1 ml was injected in the joint around the capsule. Prior to the blood injection into the joint the second needle was withdrawn from the joint (Figure 6). The procedure was repeated on the opposite side, then occlusive head bandage (Barton’s) was applied extra-orally. Post-operative mouth opening was measured (38 mm) (Figure 7). Patient was then followed on 3rd day, 15th day, 1 month, 3rd month, 6th month & for 1 year, TMJ joints were not dislocated for 1 year, no hypermobility and clicking sounds were present so there was no need to repeat the procedure in any of the joint. No postoperative dislocation or hypermobility of both the TMJ joints were noticed.
Discussion
Yawning, laughing, vomiting and excess mandibular opening during dental treatment or some medical procedures, such as endoscopies & bronchoscopies can cause the dislocation of condyle. Once the mouth is open wide, loosening of the mandibular and capsular ligaments occurs. This looseness may cause hypermobility of the mandible, which can lead to dislocation of the condyle.8
Hypermobility results when TMJ that permits excessive mandibular movements during mouth opening. It is subdivided into 2 categories: subluxation and dislocation. Some authors also introduce hyper translation as a hypermobility subgroup. Although hyper translation is characterized as an excessive opening of the mandible with the condyle moving to the most inferior portion of the articular eminence, However, patients with condyle dislocation will need to be treated because this is a condition that will hamper their daily activities.9 Most of these patients will restrain their mandibular opening when laughing, yawning because they are afraid of getting their mandible too far anteriorly to the eminence, which could cause the mandible to lock while open.10
Historically the gold standard treatment for recurrent TMJ dislocation is eminectomy, with success rates higher than 85%. It is an invasive procedure, requiring a skin incision and results in facial nerve injury and scars most of the time. Even if performed frequently with rotatory instruments, bone spicules and irregular areas may be left behind and lead to relapse.11
In 1981, Jacobi-hermanns et al. managed 19 TMJ dislocation patients with ABI, and 17 patients out of that were free of symptoms at the end of the 18-months follow up period. In 1973, Schulz treated 16 patients by injection of ABI into the affected TMJ twice a week for 3 weeks, followed by immobilization via intermaxillary fixation for 4 weeks & Patients were followed for 1-year ad patients were symptoms free at the end of 1 year follow up.12
There are various surgical modalities given in the literature as a treatment modality for recurrent temporomandibular joint dislocation. Capsular ligaments & area of articular eminence are focused, and most of them are procedures performed in patient under general anaesthesia. These surgical procedures require adequate surgical access to the TMJ area.12, 13 Autologous blood injection is an alternative to surgical modalities, minimally invasive procedure that can be performed in an outpatient basis. There is no need for incisions and tissue dissection, decreases postoperative complications such as, pain, Facial nerve injuries, unaesthetic scars and infection.
Blood is injected in pericapsular tissue and in the superior compartment of the TMJ. Bleeding will result due to insertion of a needle in the pericapsular tissue, blood coming from this wound, associated with ABI, creates a bed for fibrous tissue formation in the TMJ region. The role of blood injected in the superior compartment of the joint is still not understood fully. It is speculated that blood coming from the wounded pericapsular tissue with ABI leads to formation of adhesions in this compartment & restricted movements of the key to the success of the procedure.13, 14
Elastic bandaging provides primary clot formation, and the pain following injections will restrict mandibular movements, it permits the injected blood to settle down & creates fibrosis.15, 16 Since it is blind procedure on the basis of the success of lavage of the TMJ, (8-10) once we confirm the position of the needle to be inserted in the Articular fossa by doing protrusion of the mandible after lavage, 3 ml of blood can be safely injected in the superior compartment of TMJ. The needle is moved outward 1cm and 1 cc of blood is then injected around the pericapsular tissue.17
According to the literature, blood in the TMJ area after trauma to the condyle or after TMJ surgery, with the jaws immobilized lead to unpleasant results like asymmetry, ankylosis (fibrous or bony) of the joint. Patient should receive early attention and physiotherapy; we are creating a similar situation by injecting the blood into the joint area intentionally.18 We permitted controlled clot formation by limiting physiotherapy immediately & and Restricted mandibular movements. It is mandatory to take patient’s follow for a longer period to prevent the limited mouth-opening or trismus.19
ABI is a simple, safe, on-invasive procedure that can be done in outpatient clinic and effective for medically compromised patients or are at risk for surgical modalities. It results into fibrosis once it’s been injected into the superior compartment & around the pericapsular tissue in the TMJ.4, 20
There are few case reports in the literature which is of clinical use of the ABI, since its mechanism of action is still unclear and blood injection into the articular cavity could lead to degeneration of the articular cartilage. Until these concerns are addressed, this procedure should be avoided to be used in young population, patients with articular degeneration (rheumatoid arthritis) due to the above concerns.
Conclusions
Injections of autologous blood into the upper joint space and around the TMJ capsules bilaterally. 80% had a successful outcome and required no further treatment at their 1-year follow-up and the procedure was proven to be safe, simple, and cost effective for the treatment of chronic recurrent TMJ dislocation.