Introduction
Steroids being produced in the human body are one of the extensively advised drugs in the field of medical and dental science. Hydrocortisone, dexamethasone, methyl prednisolone, prednisolone etc. are some of the broadly used steroids for medical use. However, extra care and specific consideration is required prior to any dental treatment for patients on steroids. The misuse and risks associated with steroids have been well documented in recent times. Some of the risks related to these drugs are impaired electrolyte balance and hypertension.1 Corticosteroids have been used consistently for decades now owing to its inflammatory and immune actions. Kendall, Reichstein and Hench in 1950 were awarded with the Nobel Prize in Medicine due to their contribution in the recognition and understanding of the significance of these drugs in clinical medicine practice.2 Glucocorticosteroids are applied in oral diseases owing to their anti-inflammatory and immunosuppressive actions. The anti-inflammatory and immunosuppressive actions of steroids collectively control the defense reactions of the body.3 The typical association between physiological and pathological circumstances is intangible, even with advanced knowledge and clinical acumen. The inflammatory response is a multifaceted arrangement of proceedings triggered after almost any noxious contact to the body.2 Hence, the present review highlights on the pharmacology, pharmacodynamics and applications of corticosteroids in oral diseases.
Physiology of Corticosteroids
Corticosteroids have similarity to endogenous cortisol that is essential in protein, carbohydrate, and fat metabolism, maintenance of vascular reactivity, and body adaptability to stress.4, 5 The adrenal gland usually produces about 24-30 mg of cortisol daily, but might synthesize up to 300 mg of cortisol under stress. Cortisol secretion is controlled by the circadian rhythm (stress-related response) of the body, and is influenced by a negative feedback mechanism between the adrenals, hypothalamus, and pituitary. Corticosteroids doses of >30 mg cortisol equivalent when given for over 14 days, the hypothalamic-pituitary-adrenal axis might get inhibited and take longer time to recover. The capability to counter the stress has been shown to return within 2 weeks to 1month period. The normal secretion rate of the two principal corticoids in human is:
Hydrocortisone: 10-20 mg daily
Aldosterone: 0.125 mg daily6
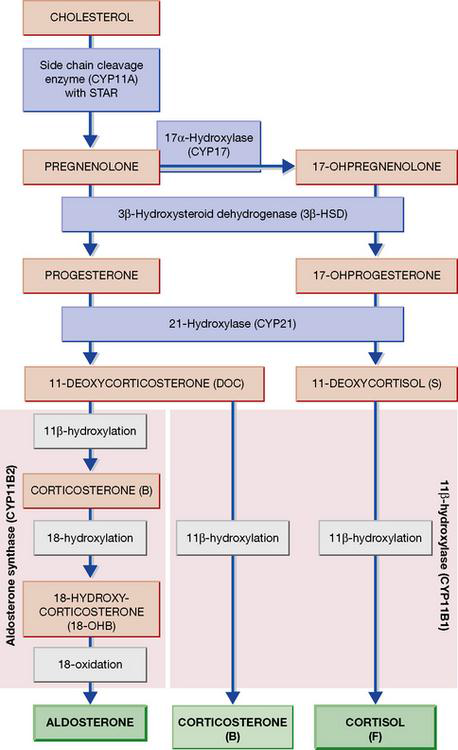
Adrenal cortex produces three groups of hormones: the glucocorticoids, androgens and mineralcorticoids (Figure 1). Glucocorticoids and steroids have extensive action on the metabolism of protein and carbohydrates. Glucocorticoids, cortisol and corticosterone and small amount of adrenal androgen and estrogens secreted by the zona fasciculate.8 Hypothalalamic pituitary axis controls these secretions via adrenocorticotropic hormone (ACTH).7
Pharmacology of Corticosteroids
Corticosteroids are classified as hydrocortisone, prednisone, triamcinolone, dexamethasone, clobetasol and mometasone. Glucocorticoids influence the metabolism of lipids, carbohydrates, proteins, calcium, and electrolytes. The pharmacological efficacy chiefly depends on the anti-inflammatory and immunosuppressive effects wherein the physiologic and metabolic effects of corticosteroids are numerous. Glucocorticoids brings inhibition of white blood cell function, lysozyme membrane stabilization, inhibits plasminogen activation, and decreases the synthesis of inflammatory mediators like prostaglandins and leukotrienes. These drugs might be directed systemically (oral and parenteral) or topically and are metabolized in the liver after conjugation and are excreted through urine.9
Mechanism of Action
The basic inflammatory signs like edema, erythema, pain and loss of function, usually occurring after difficult surgical procedure which is essential for the healing to occur. Corticosteroids helps to decrease inflammation by inhibiting phospholipase A2 (first enzyme aids in conversion of phospholipids into arachidonic acid), consequently blocking the production of prostaglandins, leukotrienes and other substances associated to thromboxane A2. Corticosteroids avert the production of these end products which is a mixture of effective inflammatory mediators and have the capability to alleviate lysozyme membranes, diminish the discharge of inflammation-causing lysozymes and reduces permeability of capillary thus preventing diapedesis. Bradykinin production which is a powerful vasodilator is also reduced.10, 11 The mechanism of action of corticosteroids is well explained in Figure 2.
Figure 2
General mechanism of action of glucocorticoids. Glucocorticoid receptor inhibition of inflammation- non-genomic activation, DNA dependent regulation & protein interference7

Anti-inflammatory action
Steroids can stabilize all biomembranes thus, elucidating their anti-inflammatory effect which in turn result in less vascular dilatation and permeability and subsequently, decreased edema, fibrin deposition, leucocyte migration and kinin formation. Due to the lysosome stabilization, discharge of hydrolytic enzyme is prohibited along with less tissue destruction. Steroids also restrain lysosomes fusion and formation of phagocytic vacuoles to decrease the phagocytosis. They have been reported to prevent prostaglandins discharge which is perhaps stabilization of cells and lysosomes since prostaglandins are formed from arachidonic acid (arising from damaged membranes). Thus this cause a decrease in the inflammatory pain that is well elucidated by the suppression of the release of several endogenous mediators, and decreased edema, and certain sensory nerve ends stimulatory factors.3
Immunosuppressive action
There are several in vitro and in vivo T-cell functions that are inhibited by steroids namely: 1) reduced lymphokine synthesis; 2) T-cells reaction against autologous tissue mostly eliminated even in physiological concentrations 3) inhibition of undefined cytolytical activity of lymphocytes against allogeneic cells. Steroids has been shown to have obscure effects on the cells that aid in immunoglobulin synthesis. Few researchers have shown an inhibition of B- and T-suppressor cell functions, while T-helper cells seem unaltered. Others have reported that suppressors are unchanged and T helpers hindered. This uncertainty might be elucidated by several types of T suppressor cells out of which few are sensitive to steroids whereas others resistant.3
Application of Corticosteroids in Oral Diseases
Corticosteroid drugs are used in various oral diseases (typified by inflammation) owing to their anti-inflammatory and suppressive actions. These drugs are used as “strong pain- killers” in the acute stage of the disease and also to control the host’s immune system for a long duration.
Oral Submucous Fibrosis (OSMF)
The anti-inflammatory action of steroid displays a direct healing effect on the mucosal patch, ulcers etc. by topical application. Steroids reduces inflammation, prevents fibrosis by decreasing the proliferation of fibroblasts and laying down collagen and help in OSMF treatment to open the mouth. Intralesional injections of dexamethasone 4 mg/ml, with hyaluronidase are prescribed once every two weeks for 20 weeks. Few other steroids advised intralesionally are triamcinolone (10 mg/ml) with hyaluronidase bi-weekly for 4 weeks. Systemic prednisone (30–40 mg/day for 14–28 days and then tapered) or hydrocortisone (100 mg/day) might be advantageous in relieving the burning sensation.9, 12
Oral Lichen Planus (OLP)
OLP may exist as reticular, papillary, atrophic, erosive, bullous, or plaque-like forms amongst which the erosive-atrophic forms are symptomatic. Steroids have been shown to play an imperative role in their symptomatic treatment.9 Some options include 0.05% clobetasol proprionate gel, 0.1-0.05% betamethasone valerate gel, 0.05% fluocinonide gel, 0.05% clobetasol ointment or cream, and 0.1% triamcinolone acetonide ointment. Triamcinolone acetonide is applied either in orabase or lozenge form. In some cases, high-potency steroid mouthwashes like disodium betamethasone phosphate, or clobetasol propionate can be applied.6 Topical steroids remaining the backbone, systemic corticosteroids have been also applied in acute exacerbation or multiple, extensive lesions.13, 14 For symptomatic treatment of OLP, 0.025% Fluocinonide, topical Betamethasone, fluticasone propionate spray, topical mometasone furoate microemulsion, clobetasol propionate in orabase, triamcinolone acetonide (mouthwash, topical, intralesional) have been used. 0.1% Fluocinolone acetonide has been established to be more efficient than triamcinolone.15 Systemic corticosteroids are used in refractory cases of erosive lichen planus [Prednisolone with its lowest effective dose – 40 to 80mg/ 6–7 days)]. For systemic steroids prescription, withdrawal must be tapered by diminishing 5 mg per week to avoid triggering any adrenal crisis.9 Systemic prednisolone is mostly recommended to control erythema and ulcers in OLP, but should be used at the lowest possible dose for minimum period (40-80 mg for 5-7 days). Oral dose of prednisone within the range of 10-20 mg/day for moderately severe cases to as high as 35 mg/day (0.5 mg/kg daily) for severe cases.6 Intra- and sublesional injections of steroids have been described to provide faster relief than topical application.3
Erythema Multiforme (EM)
It is a clinical syndrome typified by papules, macules or bullae in the skin and mucous membranes.3 Moderate-to-severe EM cases could be managed with a short course of systemic glucocorticosteroids.6 Initial treatment starts with systemic prednisone (0.5–1.0 mg/kg/day) or pulse methylprednisolone (1 mg/kg/day for 3 days).16 Intravenous pulsed dose methylprednisolone (3 consecutive daily infusions of 20–30 mg/kg to a maximum of 500 mg given over 2–3 h) is recommended, since it is considered superior because it brings about quick beneficial results as early as possible in the progression of the cutaneous insult.1 Clobetasol propionate mouthwashes in aqueous solution is applied topically.6
Pemphigus
It is a chronic autoimmune mucocutaneous disease where painful blisters are seen in the oral cavity. 0.05% fluocinoloneacetonide, or 0.05% clobetasol propionate is advised in mild Pemphigus cases whereas severe cases are advised a high dose of 100–200mg of prednisone till the symptoms regresses. This dose is steadily decreased and maintained at around 50 mg/day.9 It is evident that corticosteroid acts by interfering with lymphocyte function and reduce the antibody production.12 Systemic treatment is accompanied with a paste, an ointment, or a mouthwash. In patients deprived of any progressive oral lesions, moderate to high-potency topical corticosteroids is advised to be applied twice or thrice a day, (0.05% fluocinolone acetonide or 0.05% clobetasol propionate).17 In severe disease cases and in cases where there is dermal spread, systemic corticosteroid is recommended for treatment. Prednisolone is thought to be the first drug of choice for this disease. A total oral dose of 100-200 mg prednisolone is administered every day until clinical signs decline and then the dose can be slowly decreased to a maintenance level of 40-50 mg daily.18
Mucous Membrane Pemphigoid (MMP)
Localized and mild lesions generally react to topical steroids (triamcinolone, fluocinonide, and clobetasol propionate). Mild oral lesions are treated with topical and intralesional steroids. Desquamative gingivitis is often treated with topical steroids, however, the practitioner should keep a record for side effects (candidiasis) and other effects of systemic absorption.19 In multiple oral lesions, prednisone of 1-2 mg/kg/day is administered, with steady decreased dose, and immune-suppressors like cyclophosphamide (0.5-2 mg/kg/day), azathioprine 1-2 mg/kg/day, or mycophenolate mofetil 2-2.5 g/day have presented positive results.20
Bullous Pemphigoid (BP)
Low dose topical clobetasol propionate (10-30 g daily) has given short-term efficacy but less side-effects when compared to the high-dose topical regimen (40g daily clobetasol propionate.21 High-dose systemic corticosteroids are the regular early treatment of severe prolonged cases of BP. Early doses of prednisolone are 20 mg/day or 0.3 mg/kg/day in localized or mild disease, 40 mg/day or 0.6 mg/kg/day in moderate disease, and 50-70 mg or 0.75-1 mg/kg/day in severe disease are advised. In mild cases, clobetasol propionate cream is used; while in moderate cases, clobetasol propionate cream combined with dapsone is used (1.0-1.5 mg/kg/day) and in severe cases, oral prednisolone (0.5 mg/kg/day) may be added.22 Triamcinolone acetonide 3-10 mg/ml can be given to resistant lesions intralesionally.19
Systemic Lupus Erythematosus (SLE)
It is an autoimmune disease with immune complexes comprising of oral ulcers that are transient and occur with acute lupus flares.23 Symptomatic lesions can be repressed with topical corticosteroids.12 Oral ulcerations of lupus are short-lived and are obvious during periods of flare up. Topical betamethasone or clobetasol is advised.24 Systemic prednisone of 10–20mg/day or on alternate days might be necessaary. Intralesional triamcinolone may be beneficial in specific cases.9 Symptomatic cases can be treated with high-potency topical corticoids or intralesional steroids. Effective topical steroids and antimalarials are the chief drugs to treat SLE.25
Bell’s Palsy
Immunocompetent patients are prescribed prednisone at 1 mg/kg/day (maximum 60-80 mg) for the 1st week followed by a tapered dose in the following week.6
Ramsay Hunt Syndrome (RHS)
It is caused by the reactivation of varicella zoster virus infection. Management of these cases involves antiviral therapy and occasionally steroids. Steroid therapy is applicable for the facial paralysis in RHS. However, steroid therapy is given with caution as there exists fear of distribution of virus infection around the eyes.26
Post Herpetic Neuralgia (PHN)
This occurs after acute herpes zoster in the form of constant neuropathic pain in about 25% of patients. The constant triggering pain occurs due to the repetitive painful stimuli on the CNS resulting in central sensitization of the nociceptive system. Corticosteroids are used in such cases to treat pain and swelling and efficiently reduce PHN recurrence. Glucocorticoids are unanimously used as the chief treatment option of giant cell arteritis. This should be used directly and hostilely for suppressing inflammation and preventing vision loss and ischemic attacks.12, 26 Corticosteroids (Prednisolone) are used, which help to treat pain, swelling, and decrease the risk of PHN recurrence. A moderate dose of prednisone 40 mg daily for 10 days, with slow tapering over the following 3 weeks is an efficient method to reduce PHN incidence. Steroids along with an antiviral for simple herpes zoster cases is debatable. Steroids aid in resolution of acute neuritis and deliver an explicit development in the quality of life patients. Oral or epidural corticosteroids synchronously with antiviral therapy is efficiently used in treating moderate-to severe acute zoster, but does not affect PHN duraion.27, 28
Recurrent Aphthous Ulcers (RAU)
Steroids are recommended by many clinicians in the treatment of RAU (locally or systemically). Certain studies have reported symptomatic respite and shorter healing period, although incidence and recurrence rates are not disturbed. Similar results are observed with Levamisol® treatment (known to potentiate inflammatory and immune reactions). Steroids could limit effector B- and T-cells and T-helper cells, and Levamisol® stimulate T-suppressor cell deficiency. This suppressor cell deficiency is constant with the high antibody titres evident in RAU patients, and the reduced lymphocyte reactivity seen in some in vitro tests might reflect the same phenomenon.3
Central giant Cell Granuloma
Intracellular corticosteroid injections are recommended for non-surgical treatment. Topically, triamcinolone acetonide can also be applied as it subdues the angiogenic property of the lesion.29
Melkersson Rosenthal Syndrome
Short courses of steroids are recommended owing to its anti-inflammatory action as it is reduces swelling and persistent edema. Prednisolone in dose 1–1.5 mg/kg/day is chiefly administered. Tapering dose is initiated over 3–6 weeks depending on the severity of case and patient response.30
Temporomandibular Disorders (TMDs)
It has been established that intra-articular corticosteroids are helpful in reducing pain, swelling and dysfunction caused in TMDs.31 It might be necessary occasionally to repeat the injection, but should be done with caution for the third time, as frequent injections might reduce the recovery waiting period. In a controlled study TMJ arthritis patients, it was revealed that a single injection of methylprednisolone diluted with lidocaine might considerably decrease joint pain and other symptoms for 4-6 weeks.12, 26
Contraindications of Corticosteroids
Systemic corticosteroids should be prescribed cautiously in patients with diabetes, active peptic ulcer, uncontrolled diabetes, heart diseases, psychiatric disorders, osteoporosis, cataract, infections, glaucoma, tuberculosis, mycobacterial diseases, pregnancy, herpes simplex infection, varicella zoster infection, underactive thyroid, mental disorders and immune deficiency.32 In patients with corticosteroids hypersensitivity active tuberculosis and infections, injectable form is contraindicated. Topical corticosteroids is completely contraindicated in cases like impetigo, furuncles, erysipelas, carbuncles, cellulitis and lymphangitis.33 The safety of corticosteroids in pregnancy is still not well understood. Few studies have shown a relationship between topical corticosteroids and congenital abnormality comprising of low birth weight and oro-facial clefts. Thus, these drugs are not recommended in pregnancy.7
Side Effects of Corticosteroids
The side effects of corticosteroids use is reliant upon the treatment time period and amount of dose administered. Side effects involves weight gain, impaired growth, adrenal insufficiency, increased susceptibility to infection, myopathy, osteoporosis, osteonecrosis, fractures, glaucoma, cataract, hypertension, peptic ulcer, insomnia and diabetes. Doses in excess of 20 mg of hydrocortisone or 50 mg of prednisolone for a longer time can cause adrenal gland suppression, hence, the dose should be tapered and deferred slowly.34
Conclusion
Corticosteroids usage being very fundamental for the management of several oral diseases, have also been used to reduce the post-operative illnesses like edema and pain especially after oral surgical procedures. Due to their distinctive characteristic anti-inflammatory and anti-allergic actions, corticosteroids have established their largest application in the management of acute and chronic conditions. Nonetheless, these drugs exhibit some side effects which might sometimes be severe and life threatening hence, any positive outcome from them should always be considered keeping in mind the prospective risks for the patient. It is imperative to advise and prescribe the least powerful type of corticosteroids and a minimum dose essential to establish a specific therapeutic effect it is also to be noted that the use of non-steroidal agents to lessen the corticosteroid dose and also giving corticosteroids for a small time period are few methods to decrease the hostile effects of these drugs. The extensive application of corticosteroids renders it as the “life-protecting hormone” and aldosterone is referred to as the “life-saving hormone.” It can thus be concluded that corticosteroids play a significant role in the of lesions affecting the oral mucosa and skin. In addition, its importance in medical emergencies cannot be neglected.