- Visibility 254 Views
- Downloads 15 Downloads
- DOI 10.18231/j.jooo.2022.005
-
CrossMark
- Citation
Treatment efficacy using occlusal splint for anterior disc displacement without reduction of temporomandibular joint
- Author Details:
-
Nimisha Divakar *
-
Manoj Vengal
-
Auswaf Ahsan
Introduction
Temporomandibular joint where temporal bone associates with mandible, is most complex joint in human body[1]
Temporomandibular disorders are defined as ‘Subgroup of craniofacial pain problems that involve the TMJ, masticatory muscles, and associated head and neck musculoskeletal structures[2] Internal derangement in temporomandibular joint (TMJ) is a common dysfunction of the head and neck area. According to classification of Research Diagnostic Criteria for Temporomandibular disorder s there are three main types of internal TMJ derangement: disc displacement with reduction and disc displacement without reduction with or without limited mouth opening. The most common type is disc displacement with reduction characterized by clicking in the TMJ.[2] Pain in affected joint and restricted mouth opening (≤ 40 mm) are the common symptoms of anterior disc displacement without reduction which results in decreased function and insist the patient to seek professional help.[3] Parafunctional habits, anatomical factors, trauma or general hypermobility of the joints can cause this. Mostly, articular disc is displaced anteriorly, blocking translating movement of the condyle, causing restricted mouth opening. In addition the bilaminar zone becomes overloaded by direct contact with the condyle, which is the main reason of pain in the TMJ.[4]
Anterior disc displacement without reduction is usually a self-limiting, benign condition, but it may lead to osteoarthritis. Accordingly, if there is no significant improvement after 12 weeks of following natural course of disc displacement without reduction, treatment should be implemented.[5] In the treatment protocol, initial therapy should be minimally invasive. The surgical methods of treatment should be considered only after 6 months of unsuccessful conservative management.[6]
Etiologic variants of TMDs revolved mostly around theories of occlusal disharmonies and/or skeletal malalignments, where dentists became almost exclusively responsible for their management and oral appliances became a major treatment modality for temporomandibular disorder patients. Now also, oral apliances are TMJ deprogrammers which alleviates pain and reimpose proper function by producing occlusal insularism, relaxing jaw musculature, restoring vertical dimension of occlusion by unloading the joint(s), or TMJ repositioning.[7] Occlusal appliances commonly used for temporomandibular disorders are Flat stabilisation appliance, Pivot appliance, Anterior bite plane, Posterior bite plane, Hydrostatic appliance, Minianterior appliance and Anterior repositioning appliance.[8] Management of TMDs with occlusal splint is a reversible, non- invasive modality which causes minimum damage to tissues, when compared to other irreversible treatment modalities. This makes this study relevant.
Aim and Objectives
To assess the effectiveness of occlusal splint in patients with anterior disc displacement without reduction by evaluating,
Reduction in pain
Improvement in mouth opening.
Materials and Methods
Subjects included in this quasi- experimental study were taken from Out-Patient Department of Oral Medicine and radiology, who had been diagnosed with ADD without reduction during the period 2016 to 2018, according to RDC/TMD criteria in the age group 16 – 55 yrs. Patient concern was obtained before the study began and study was approved by Institutional review board (KMCTDC/IEC/2016/24).
Inclusion criteria: (any 5 out of 7)
Persistent limited mouth opening with sudden onset
History of TMJ clicking in affected joint that ceases with locking
Straight line deflection to affected side on mouth opening
Impaired lateral movements towards the contra lateral side
TMJ pain related to mouth opening and chewing
Pain on palpation of the affected joint
Evidence of condyle movement restriction on the affected side during mouth opening assessed by palpation and radiology.
Exclusion criteria
Systemic diseases that leads to derangement
Other types of treatment attempts by other providers during previous year
Insufficient compliance
Loss of follow up
Sample size calculation
The sample size is calculated using the formula,
n=(Zα + Zβ) 2 (S.D) 2d 2(One group pre-test / post-test study)Patients diagnosed with ADD without reduction were evaluated by the questionnaire.
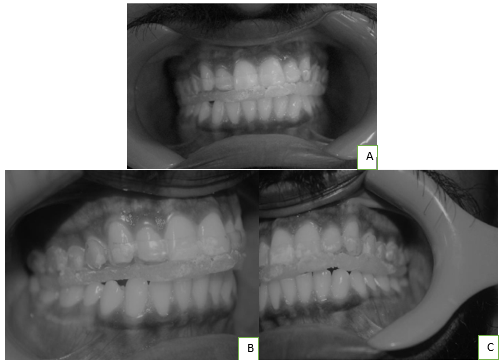
Maximum mouth opening with and without pain was measured using calipers. Intensity of pain was evaluated using VAS. Patient instructed with conservative management methods like hot and cool fomentation, muscle exercises, soft diet and muscle relaxants if necessary. After taking consent, impression of maxillary arch was made. A working cast is withdrawn from the impression and excess stone is removed leaving a proper replica of maxillary teeth and palate till the vestibule. A 2mm hard vaccum former sheet is adapted to the cast using a pressure adapter and trimmed to desired shape ([Figure 4]). Reevaluation of pain and mouth opening will be done in the second visit. After checking the fitting of appliance, 1mm thickness self-cure acrylic added to the surface thus filling the indentations on the occlusal surface of the appliance and making even contact. The occlusal adjustments also done in the same appointment. After achieving equal contact in all the teeth in the flat occlusal surface, splint is delivered ([Figure 5]). Patient was instructed to wear the splint 24 hrs except while eating. A pamphlet containing the instruction to use the splint will be given to the patient. Patient was instructed to return whenever they have any difficulties or else recalled after 4 weeks. On the third visit, which was 1 month after the splint delivery, the splint is removed. Clinical examination of TMJ will be done. Pain intensity and maximum mouth opening will be measured.


Statistical analysis
Results were compared using paired‘t’ test if the data obtained after the analysis were in normal distribution. If the data is not in normal distribution, Wilcox on signed rank test or Shapiro- Wilk test was used. P value < 0.05 is considered significant. SPSS version 20 software is used.
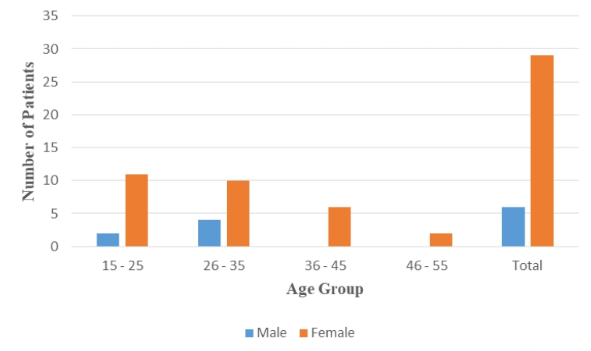
|
Age (years) |
Gender |
|
|
Male |
Female |
|
|
15 – 25 |
2 |
11 |
|
26 – 35 |
4 |
10 |
|
36 – 45 |
0 |
6 |
|
46 - 55 |
0 |
2 |
|
Total |
6 |
29 |
|
|
|
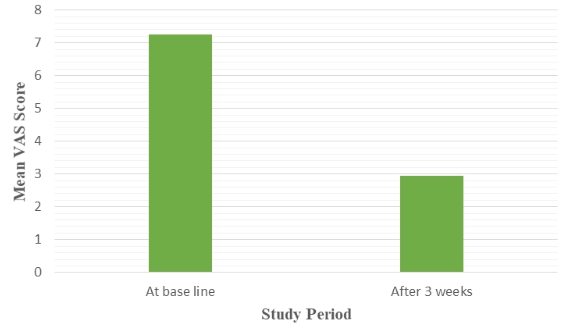
Mean |
Std. Deviation |
p value |
|
VAS before |
35 |
7.26 |
0.886 |
p < 0.001* |
|
VAS after |
35 |
2.94 |
1.413 |
|
|
Difference in score |
- 4.314 |
1.5487 |
|
|
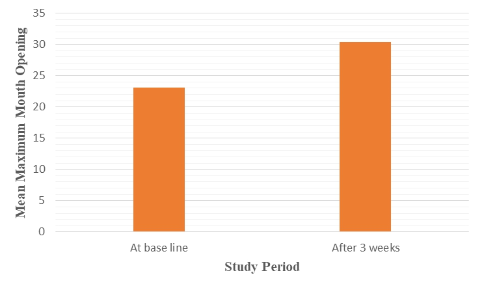
|
Mean |
Std. Deviation |
p value |
|
MMO before |
35 |
23.09 |
4.252 |
p< 0.001* |
|
MMO after |
35 |
30.37 |
5.435 |
|
|
Difference in score |
7.2857 |
4.0335 |
Results
Thirty eight patients were participated in the study. 3 of them could not complete the study due to various reasons. (2 patients discontinued the therapy, 1 patient had broken the splint). Amongst the subjects selected for the study, 82.8 % were females and 17.1% were males, mostly in the age group of 15-35. ([Table 1]). Data were tested for normality. As there is significant variation in values, the data did not follow a normal distribution. So, paired t test cannot be used for the analysis.
The Wilcoxon signed rank test was used for the statistical evaluation of change in pain and for the evaluation of change in maximum mouth opening before and after treatment. The mean Visual Analog Scale (VAS) score before treatment was 7.26 ±0.88. After treatment with splint therapy, VAS score was reduced to 2.94 ±1.41. The difference in VAS score was 4.314 ± 1.54, which is highly significant statistically ([Table 2],[Figure 6]).[Table 3] shows the mean value of maximum mouth opening before treatment was 23.09 ±4.25. After treatment with splint therapy, it was increased to 30.37±5.43. The difference in mouth opening was 7.28 ± 4.03, which is highly significant statistically. ([Table 3])
Discussion
The present study evaluates the treatment efficacy of occlusal splint for the treatment of anterior disc displacement without reduction of temporomandibular joint. The parameters evaluated are the pain in the TMJ region and maximum mouth opening.
The male — female ratio of the 35 patients who completed the study was 1:4.8. This indicates the increased prevalence of temporomandibular joint disorders in females when compared to males. The predilection for females to develop TMJ disorders has already been established in several earlier studies.[9], [10], [11], [12], [13] LeResche suggests that these gender discrepancies may be related to the presence of reproductive hormones.[14] Prevalence of myofacial pain is more in women with childbirth experience indicating the role of reproductive hormones in TMDs.[15] However, it should be noted that Sylvester et al. found a similar prevalence in men and women.[16] But, there are certain contradictory studies propose that there are no statistically significant gender differences in the actual incidence of changes in joint problems. Meisler stated that the pain onset tends to occur after puberty and reaches its peak in the reproductive years and risk of TMD appears to be increased with increasing doses of estrogen.[17] According to Kuttila et al., the highest prevalence occurs in women aged 20 – 40 years, with the lowest being among children and elderly due to high stress scores in women.[18] Primary aim of this study was not to evaluate the prevalence of any particular age or gender, but it is mentioned here since the same was reported in several earlier studies. Temporary occlusal splint therapy with a vertical height exceeding the physiologic rest position does not cause increase in tonus or hyperactivity of jaw muscles, but increases vertical dimension of occlusion since they can be adjusted with a vertical height that exceeds the physiologic inter-occlusal distance.[19] Splint therapy decreases the level of muscle activity by unloading of the joint.[20] Splint therapy allows the condyles to seat in centric relation. For the condyles to seat completely under the disc in antero-superior position, the superior belly of lateral pterygoid should obtain its full extension.[21] An ideal splint with proper extensions gives a proper occlusal harmony and articular disc obtain its anterosuperior position over condylar head thus smoothening the muscles.[22] Occlusal forces are distributed equally through the masticatory system by these appliances but its intensity not reduced. Episodes of bruxing can be reduced by splint.[23] Occlusal splints insist the patient to position his mandible in new posture. It leads to a new articular and muscular balance.[24] It will take time for the patient to get acclimatize to this new posture so clenching will be reduced thus protecting TMJ.[25] When occlusal disharmony causes hyper activation of muscles and excursive mandibular movements, it causes pain. A proper splint has even contacts in the occlusal surface causing immediate disclusion of all posterior teeth by the anterior guidance and condylar guidance in all movements, soothens the muscle and alleviates the pain.[26]
There are several non- dental reasons for the effectiveness of occlusal splint therapy. The increased cognitive awareness of the patient regarding the positioning and use of the jaw, the change in oral tactile stimuli, and the decrease in oral volume can all influence the patient to learn what position or activities are harmful.[27] It provides a placebo effect. Proprioceptive fibers in tooth supporting apparatus send message to central nervous system, triggering muscle patterns that protect them from overload. An equal force dissipation over large surface area balances the load and allows for muscle symmetry.[28] Zhang et al. conducted a meta-analysis of 13 studies and stated that maximum mouth opening was increased and pain intensity was reduced.[29] And Friction et al., after doing a meta-analysis and systematic review of 47 publications citing 44 RCTs presented results in favour of occlusal splint, but pointed out limitations regarding the type of TMDs origin and duration of therapy.[30] Ekberg et al. stated that the positive treatment outcome obtained by use of a stabilization appliance to alleviate the signs and symptoms in patients with temporomandibular disorders persisted after 6 and 12 monthsc.[31] Nitecka-Buchta et al. used VAS for the evaluation of pain in the TMJ in 35 patients having temporomandibular disorders before and after muscle stretching with occlusal splint therapy. They concluded that pain intensity is reduced significantly afterwards.[32] Maximum mouth opening was increased by 8.5 mm along with reduced pain intensity in 20 patients treated with stabilisation splint compared to the control group of 20 patients treated with pivot appliance, in a study conducted by Stiesch‐Scholz et al. in 2005.[33] A two year follow up study proved that there was significant improvement in the maximum mouth opening and complaint of pain.[34] In a randomised control study by Wahlund et al., after a 6-month occlusal appliance therapy in 64 adolescents of age 12-19 years, there was significantly higher reduction in frequency of pain, in pain intensity and in a composite pain index for patients treated with OA compared with control group[35]
There are certain studies, the results of which are inconsistent with this present study. Based on the study results of Moloney et al., even in experienced specialist hands, anterior repositioning splint therapy is not likely to be successful in maintaining the recaptured disc in more than 36 per cent of patients in the long-term.[36] In the study by Lundh et al. for the short term, occlusal splint was effective in reducing the pain intensity and increasing mouth opening. But on the long term follow-up, there was no statistically significant benefit of a flat occlusal splint over non-treatment control subjects.[37] Though present study was highly significant statistically, the results are only applicable for a short duration. Whether or not, these results last beyond 3 months is not discernible since follow up could not be continued beyond that period. A randomized, controlled clinical trial was conducted by Haketa et al. comparing the therapeutic effects of splint and joint mobilization self-exercise on ADD without reduction but the results showed maximum improvement in the exercise group.[38] More precise customised occlusal splints can be fabricated incorporating jaw tracking, CBCT and digital impression. Aslanidou et al. fabricated a customised occlusal splint incorporating SiCAT software. Anatomical position of the articulating components were visualized along with assessment of mandibular movements and all the data were sent to SiCAT and a customized occlusal splint was manufactured thus opening new possibilities and potentials for the management of temporomandibular disorders.[39]
The limitations of this study are, small sample size, short duration and having used a manual method for registration of centric relation. A more accurate method like face bow can be used to register centric relation, which may give superior results. The use of CBCT imaging and SiCAT in the study can improve the validity of the study by incorporating the finer aspects of mandibular movement in the design of the splint.
The success of a treatment modality for TMD relies upon two considerations: relieving the symptoms and treating the cause. In this view, various treatment modalities have been tried for temporomandibular joint disorders over time. But, no single treatment modality has been proven to be better than any other. Based on its non-invasiveness, reversibility and conservative nature, occlusal splints are an important part of internal derangement treatment. However, relief of symptoms provided by splint therapy is of a temporary nature. Therefore, a permanent solution is needed following treatment with an occlusal splint.
Conclusion
The aim of the study was to assess the effectiveness of flat occlusal splint in patients with ADD without reduction by assessing pain and difficulty in mouth opening before and after treatment.
35 patients were included in the study and results showed that there is a significant reduction in the pain and significant improvement in the mouth opening after using flat occlusal splint.
Since the study was done for a short duration, results only indicate efficacy for a short term. However, further studies are needed on a long term basis.
Acknowledgment
We would like to thank patients, nursing staffs and dental assistants who helped us to fulfill the study. Also, to our colleagues and other faculties for their immense help. No fund has been taken for this research.
Source of Funding
None.
Conflict of Interest
None.
References
- S J Scrivani, A David, L B Keith. Temporomandibular disorders. New Engl J Med 2008. [Google Scholar]
- E Schiffman, R Ohrbach, E Truelove, J Look, G Anderson, J P Goulet. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache 2014. [Google Scholar] [Crossref]
- M Kreiner, E Betancor, G T Clark. Occlusal stabilization appliances: evidence of their efficacy. J Am Dent Assoc 2001. [Google Scholar] [Crossref]
- J P Okeson. Management of temporomandibular disorders and occlusion. 2014. [Google Scholar]
- A L Young. Internal derangements of the temporomandibular joint: A review of the anatomy, diagnosis, and management. J Indian Prosthodont Soc 2015. [Google Scholar] [Crossref]
- M Miernik, W Więckiewicz. The Basic Conservative Treatment of Temporomandibular Joint Anterior Disc Displacement without Reduction. Adv Clin Exp Med 2015. [Google Scholar] [Crossref]
- R Emshoff. Clinical factors affecting the outcome of occlusal splint therapy of temporomandibular joint disorders. J Oral Rehabil 2006. [Google Scholar] [Crossref]
- G D Klasser, C S Greene. Oral appliances in the management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009. [Google Scholar] [Crossref]
- T Y Kim, J S Shin, J Lee, Y J Lee, M R Kim, Y J Ahn. Gender difference in associations between chronic temporomandibular disorders and general quality of life in Koreans: a cross-sectional study. . PloS one 2015. [Google Scholar]
- B Bagis, E A Ayaz, S Turgut, R Durkan, M Özcan. Gender difference in prevalence of signs and symptoms of temporomandibular joint disorders: a retrospective study on 243 consecutive patients. Int J Med Sci 2012. [Google Scholar] [Crossref]
- M P Warren, J L Fried. Temporomandibular disorders and hormones in women. Cells Tissues Organs 2001. [Google Scholar] [Crossref]
- P Currie. Age and gender as factors in temporomandibular joint movement in adolescents, as determined by computerized 3D electronic condylography.. Int J Stomatology Occlusion Med 2010. [Google Scholar] [Crossref]
- A L Witzel, J E Costa, M C Bolzan, M L Carli, T B Nunes, Di Matteo. Correlation between gender, temporomandibular joint disc position and clinical findings in patients with temporomandibular disorder. Med Expr 2015. [Google Scholar] [Crossref]
- L Leresche, K Saunders, V Korff, M R Barlow, W Dworkin. Use of exogenous hormones and risk of temporomandibular disorder pain. Pain 1997. [Google Scholar] [Crossref]
- T T Dao, K Knight. Ton-That V. Modulation of myofascial pain by the reproductive hormones: a preliminary report. J Prosthet Dent 1998. [Google Scholar] [Crossref]
- D Sylvester, E Exss, C Marholz, R Millas, G Moncada. Association between disk position and degenerative bone changes of the temporomandibular joints: An imaging study in subjects with TMD. J Craniomandibular Pract 2011. [Google Scholar] [Crossref]
- J G Meisler. Chronic pain conditions in women. J Womens Health 1999. [Google Scholar] [Crossref]
- M Kuttila, P M Niemi, S Kuttila, P Alanen, L Bell. TMD treatment need in relation to age, gender, stress, and diagnostic subgroup. J Orofacial Pain 1998. [Google Scholar] [Crossref]
- A Manns, R Miralles, H Santander, J Valdivia. Influence of the vertical dimension in the treatment of myofascial pain-dysfunction syndrome. J Prosthetic Dent 1983. [Google Scholar] [Crossref]
- A Manns, R Miralles, F Cumsille. Influence of vertical dimension on masseter muscle electromyographic activity in patients with mandibular dysfunction. J Prosthetic Dent 1985. [Google Scholar] [Crossref]
- M Schmitter, M Zahran, J M Duc, V Henschel, P Rammelsberg. Conservative therapy in patients with anterior disc displacement without reduction using 2 common splints: a randomized clinical trial. J Oral Maxillofac Surg 2005. [Google Scholar] [Crossref]
- R Srivastava, B Jyoti, P Devi. Oral splint for temporomandibular joint disorders with revolutionary fluid system.. Dent Res J 2013. [Google Scholar]
- K Holmgren, A Sheikholeslam, C Riise. Effect of a full-arch maxillary occlusal splint on parafunctional activity during sleep in patients with nocturnal bruxism and signs and symptoms of craniomandibular disorders. J Prosthetic Dent 1993. [Google Scholar] [Crossref]
- A Jokstad, A Mo, B S Krogstad. Clinical comparison between two different splint designs for temporomandibular disorder therapy. Acta Odontol Scand 2005. [Google Scholar] [Crossref]
- P Rèj, C Perez, L Darmouni, J F Carlier, J D Orthlieb. The occlusal splint therapy. J Stomat Occ Med 2009. [Google Scholar]
- E H Williamson, D O Lundquist. Anterior guidance: its effect on electromyographic activity of the temporal and masseter muscles. J Prosthet Dent 1983. [Google Scholar] [Crossref]
- S S Adibi, E I Ogbureke, B B Minavi, K U Ogbureke. Why us e oral splints for temporomandibular disorders (TMDs). Tex Dent J 2014. [Google Scholar]
- R Srivastava, J B Dixit, J Arya, A Samant. NTI-tss®-A Novel Approach To The Management Of Temporomandibular Joint Disorders. J Clin Dent Res Edu 2013. [Google Scholar]
- C Zhang, J Y Wu, D L Deng, B Y He, Y Tao, Y M Niu. Efficacy of splint therapy for the management of temporomandibular disorders: a metaanalysis. Oncotarget 2016. [Google Scholar] [Crossref]
- J Fricton, J O Look, E Wright, A Jr, F G Chen, H Lang. Systematic review and meta-analysis of randomized controlled trials evaluating intraoral orthopedic appliances for temporomandibular disorders. J Orofacial Pain 2010. [Google Scholar]
- Ekberg, D Vallon, M Nilner. Occlusal appliance therapy in patients with temporomandibular disorders. A double blind controlled study in short term perspective. Acta Odontol Scand 1998. [Google Scholar]
- A N Buchta, B Marek, S Baron. CGRP plasma level changes in patients with temporomandibular disorders treated with occlusal splints-a randomised clinical trial. Endokrynologia Pol 2014. [Google Scholar] [Crossref]
- M S Scholz, J Kempert, S Wolter, H Tschernitschek, A Rossbach. Comparative prospective study on splint therapy of anterior disc displacement without reduction. J Oral Rehabil 2005. [Google Scholar] [Crossref]
- S Sato, H Kawamura, H Nagasaka, K Motegi. The natural course of anterior disc displacement without reduction in the temporomandibular joint: follow-up at 6, 12, and 18 months. J Oral Maxillofac Surg 1997. [Google Scholar] [Crossref]
- K Wahlund, I M Nilsson, B Larsson. Treating temporomandibular disorders in adolescents: a randomized, controlled, sequential comparison of relaxation training and occlusal appliance therapy. J Oral Facial Pain Headache 2015. [Google Scholar] [Crossref]
- F Lundhoney, J A Howard. Internal derangements of the temporomandibular joint. III. Anterior repositioning splint therapy. Aust Dent J 1986. [Google Scholar] [Crossref]
- H Lundh, P L Westesson, L Eriksson, S L Brooks. Temporomandibular joint disk displacement without reduction: Treatment with flat occlusal splint versus no treatment. Oral Surg Oral Med Oral Pathol 1992. [Google Scholar] [Crossref]
- T Haketa, K Kino, M Sugisaki, M Takaoka, T Ohta. Randomized clinical trial of treatment for TMJ disc displacement. J Dent Res 2010. [Google Scholar] [Crossref]
- K Aslanidou, C H Kau, C Vlachos, T A Saleh. The fabrication of a customized occlusal splint based on the merging of dynamic jaw tracking records, cone beam computed tomography, and CAD-CAM digital impression. J Orthodont Sci 2017. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Divakar N, Vengal M, Ahsan A. Treatment efficacy using occlusal splint for anterior disc displacement without reduction of temporomandibular joint [Internet]. J Oral Med Oral Surg Oral Pathol Oral Radiol. 2025 [cited 2025 Sep 03];8(1):20-26. Available from: https://doi.org/10.18231/j.jooo.2022.005
APA
Divakar, N., Vengal, M., Ahsan, A. (2025). Treatment efficacy using occlusal splint for anterior disc displacement without reduction of temporomandibular joint. J Oral Med Oral Surg Oral Pathol Oral Radiol, 8(1), 20-26. https://doi.org/10.18231/j.jooo.2022.005
MLA
Divakar, Nimisha, Vengal, Manoj, Ahsan, Auswaf. "Treatment efficacy using occlusal splint for anterior disc displacement without reduction of temporomandibular joint." J Oral Med Oral Surg Oral Pathol Oral Radiol, vol. 8, no. 1, 2025, pp. 20-26. https://doi.org/10.18231/j.jooo.2022.005
Chicago
Divakar, N., Vengal, M., Ahsan, A.. "Treatment efficacy using occlusal splint for anterior disc displacement without reduction of temporomandibular joint." J Oral Med Oral Surg Oral Pathol Oral Radiol 8, no. 1 (2025): 20-26. https://doi.org/10.18231/j.jooo.2022.005
