Introduction
Tori are normal anatomic variations of bony exostoses, which are usually present on the mid- hard palate or mandible on lingual region.1, 2 Torus mandibularis (TM) are usually bilateral (90%), symmetrical and lingually present.2 They are mostly asymptomatic but may grow to large sizes and can cause discomfort.2 Clinically TM may occur as hard growth, single or multiple, unilaterally or bilaterally, in dentulous or edentulous jaw. Mandibular tori are mostly small in size.2 Their function is questionable and they may hinder during intraoral radiography or prosthesis placement. The prevalence of torus mandibularis varies from 1%-64%. Torus mandibularis are more common in males and are rare before the first decade of life. Tori are mostly seen in young adults and middle-aged individuals which suggests role of the environmental and functional factors such as masticatory functional stress as etiological factors, along with genetic causes.1 Functional stress may release bone morphogenic proteins resulting in osseous growth at stress site.2 Although its etiology is unclear, 30% are attributed to genetics and 70% to environmental causes.1, 2 Tori are not removed in most of the cases, as they are benign and asymptomatic. Surgical removal is advised in cases of mucosal trauma, ill-fitting prostheses, interference with denture impressions or dental appliance placement, restricted tongue space, obstructive sleep apnea and difficulty in speech occurring in association with tori. They can also hinder laryngoscopy or endotracheal intubation.2, 3 We present an unusual case of large bony exostosis on the lingual aspect of the mandible with features resembling TM and osteoma with review of the literature.
Case Report
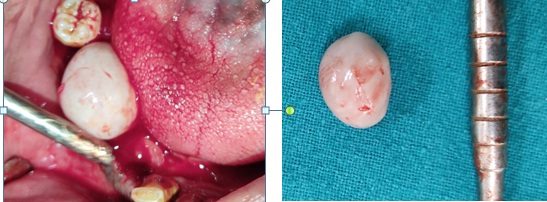
A 46-year-old male patient complained of intraoral swelling for 20 years which had gradually increased in size. He also gave history of discomfort while chewing. On examination an oval shaped nodular growth of size approximately 1.5 x 1 cm was seen on the right side of the floor of the mouth, covered with normal mucosa. Growth was pedunculated, hard, non-tender and attached lingually to the edentulous mandible in the alveolar region. Provisional diagnosis of benign tumor of the bone was given and differential diagnosis of mandibular tori, osteoma and peripheral ossifying fibroma was considered. CBCT revealed a well defined pedunculated hyperdensity with smooth surface, lingual to right premolar alveolus crest region. Nodule showed normal trabecular bone appearance centrally surrounded by well-defined cortical margin. Approximate measurements at it’s greatest dimension in axial view were 15.23mm x 12.71mm and coronal view were 13.32mm x 10.56mm. (Figure 1) The surgical excision was performed under local anaesthesia and the growth was excised in toto. Histopathologic examination confirmed provisional diagnosis of torus mandibularis and it revealed mature lamellar bone interspersed with fibrous marrow tissue. Osteocytes were evident within lacunar spaces in the bone with no inflammatory cell infilteration. (Figure 2) Thus final diagnosis of torus mandibularis was given. The six months follow up revealed no evidence of recurrence of the TM.
Discussion
Sclerotic lesions of the jaws are common and are often encountered on radiographs and computed tomography (CT). They can be classified radiographically into odontogenic, non-odontogenic and mixed lytic sclerotic lesions.4 Our case presented non-odontogenic sclerotic lesion of the mandible. Imaging plays a pivotal role in diagnosis of sclerotic lesions of the jaws. If a lesion is in approximation to the tooth then it is most likely to be an odontogenic pathology otherwise it is a non- odontogenic pathology. Imaging is significant in understanding density, location, periphery, internal structure and relationship with dentition. These characterizations along with demographic details may assist in giving a particular diagnosis or differential diagnosis specifically for benign bony lesions.4
Osteomas are benign, slow growing defined osteogenic lesions characterised by proliferation of compact or cancellous bone. They are categorised into endosteal, peripheral or extraskelatal types. Peripheral osteoma of the craniofacial region occurs most frequently in the paranasal sinuses. and rarely jaws. Common site of involvement is the lingual aspect, angle and inferior border of the mandible than the maxilla.5, 6 Tori are non pathological bony outgrowths with a natural occurrence. It often occurs adjacent to the bicuspids above the mylohyoid attachment.2 MT are often diagnosed incidentally in 4th decade during clinical examination.7 Diagnosis of MT or Osteoma is still debatable as both are benign bony exostosis. They show very similar clinical and radiographic features or MT could be considered as type of osteoma which is present as benign bony growth or exostosis in mandible at lingual site of bicuspids.1, 2, 5, 6
Previous studies on fetuses, suggested that there is a constant bony prominence at birth, adjacent to the mental foramen. This bony growth, at the origin of the mandibular torus appears, if during fetal development the mandibular internal lamina reaches the posterior and upper part of the Meckel cartilage. The occurance of tori also depends on ethnic groups, with higher frequencies in Eskimos, Japanese, spanish, Ghanian, Americans, Caucasian and Asian populations.2, 7 Literature suggests that post excision recurrence of the benign bony exostosis is not seen.1, 2, 5, 6 A case report also revealed local recurrence of the lesion after one month in a male patient, which was surgically excised again. Bruxism is a likely explanation for the early recurrence in this case as no reappearance of the exosotosis was observed after using a mouth guard.7 An association has been found between abraded teeth, parafunctional habits and occurance of torus mandibularis.1 A high prevalence of mandibular tori has also been reported in systemic disorder such as primary hyperparathyroidism8 and in younger age group with a higher blood phosphate level in hemodialysis patients.9 Similarly in our case, the patient had partially edentulous jaws and was not using any prostheses and this could be one reason for increased occlusal stress. Diagnosis of the TM is mostly clinical, and biopsy is generally not necessary. Differential diagnosis of osteoma, peripheral ossifying fibroma, osteoid osteoma, and osteoblastoma should be considered in a unilateral, slow -growing lesion. Surgical removal should be advised in case of continuous growing pathology or in case of discomfort and regular follow up should be done postoperatively to rule out recurrence of the lesion.
Conclusion
Large mandibular tori or peripheral osteoma of the jaws are relatively rare. Oral physicians and oral sugeons should evaluate characteristic features of benign sclerotic jaw lesions and differential diagnosis for the same. Based on clinical and radiological features, the dentist can determine whether the lesion should be left untreated with regular follow up or be approached surgically for removal. Further research should be done to evaluate the role of occlusal stress in occurrence of tori and it will assist in management of such cases.