Introduction
The prevalence of CRF with T2DM is becoming a major public health problem with high number of cases in India. CRF patients with superseded diabetes are prone for oral infection.1 These patients are immuno-compromised and their salivary flow tends to slow. When the immune system is suppressed, microbial agents of normal oral flora have an opportunity to become pathogenic, which causes infection and destruction of the oral cavity. Generally, the reported oral lesions in systemic illness include periodontitis, white patches, red patches, mucositis, and oral candidiasis, burning sensation, abnormal salivary flow rates and pigmentation.2 The presence of these specific lesions indicate systemic diseases.3 However significant improvement has been reported following treatment of associated oral lesions.
A wide range of oral signs and symptoms such as dry mouth, change in taste, pallor, uremic fetor and dental calculus have been reported. The patients of CRF undergoing hemodialysis showed poor oral hygiene and higher prevalence of periodontal disease.4, 5
The National kidney foundation (NKF) defined chronic kidney disease as kidney damage for three or more months associated with structural or functional abnormalities of the kidney, with or without decreased glomerular filtration rate.6 The clinical findings in CRF patients are essentially as stated oral lesions in systemic diseases, unfortunately, attention to the oral aspects has been lacking. Increase in systemic inflammatory burden which worsens the underlying systemic disease are consequences of untreated oral lesions in CRF with T2DM.3 Hence attempt was made to study the Oral and dental manifestations in chronic renal failure with type 2 diabetic patients receiving hemodialysis.
Materials and Methods
Study design
This study was conducted at Department of Oral Pathology, Vydehi Institute of Dental sciences and Research Centre, Bangalore. Patients who were clinically diagnosed cases of chronic renal failure with Type 2 diabetes reported to the department of Nephrology at Vydehi medical college hospital, Bangalore were considered for the study. Ethical clearance was obtained from the institutional ethical committee for human experimentation as per standard guidelines and informed consent was obtained from all the individuals.
Subjects
It is a hospital based case control study consisting of 51 individuals including 24 cases of Chronic renal failure with type 2 diabetes mellitus (CRF with T2DM group) and 27 healthy individuals, age and sex matched individuals were randomly selected as healthy control group. Detailed Oral examination of all the individuals were carried out using diagnostic instruments.
Data collection
Demographic data as well as details such as fasting blood sugar level, post prandial blood sugar, glycated hemoglobin level (HbA1c level), duration of the diabetes and medication taken were recorded. The patients of diabetes were divided into 3 groups according to their glycemic index; No diabetes (HbA1c <5%) controlled diabetes (HbA1c ≤5%), and Uncontrolled diabetes (HbA1c ≥7%). Patients subjected to radiotherapy / chemotherapy, Patients on any long term medications like systemic corticosteroids, antibiotics, and immunomodulants, patients wearing dentures were excluded from the study.
Clinical examination
Healthy controlled subjects were made to sit comfortably on a dental chair and were examined under artificial illumination and were examined bedside for patient convenience. The clinical examination was carried out as described by Kerr, Ash and Millard.7 Intraoral examination was performed to evaluate oral manifestations in both the groups and the findings were recorded in pre designed proforma. Both the groups underwent laboratory examinations.
Laboratory investigations
Hematological profile: Hemoglobin estimation, Blood urea, serum creatinine and serum albumin estimation were performed by automated analyzer. The results were recorded and tabulated.
Biochemical tests
Glycated hemoglobin HbA1C : The HbA1c levels were determined by the borate affinity assay (Nycocard Axis-shield PoC AS, Norway) Briefly 2 ml of blood was collected in an ethlenediamine tetracetic acid tube and HbA1c levels were assayed as per instructions supplied with the kit.8
Statistical analysis
Data obtained were computed on Microsoft excel sheet. Statistical analysis was carried by using Statistical package for social sciences (SPSS version 17.0, Chicago, USA) and Graph pad prism version 5.0. Descriptive statistics, bivariate analysis using student t test and chi-square test were used to compare two groups. Data expressed as mean ± SD. The level of significance of study parameters on categorical scale between the groups. P value: <0.05 was considered statistically significant.
Results
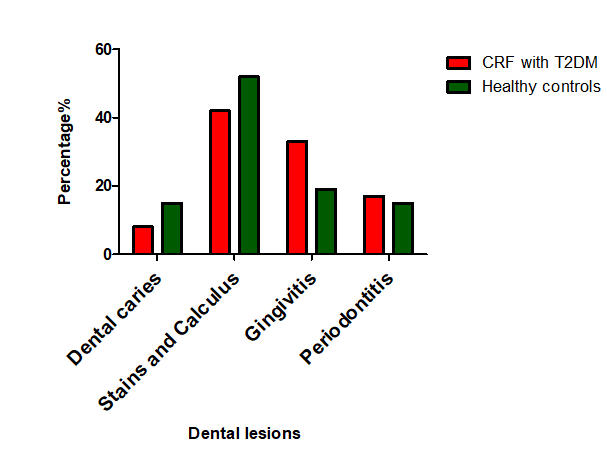
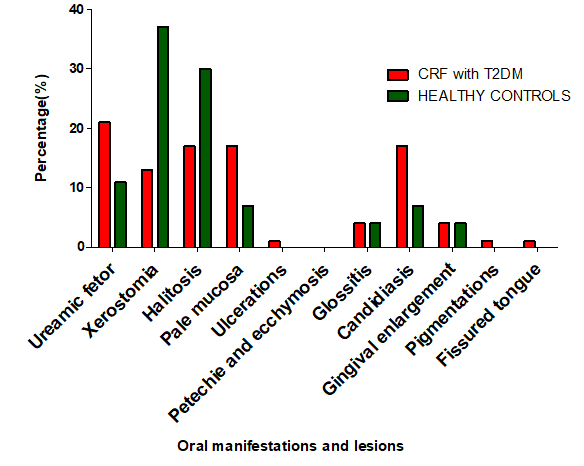
51 CRF with T2DM and healthy patients participated in this study of which 28(54%) were males and 23(45%) were females. The mean age group of the male and female patients were 52.1±8.8 and 48.6±5.3 respectively (Table 1). The average duration of diabetes of the male patients were 15.2 ±6.4 years and the female patients were 13.6±2.5 years (Table 1). CRF with T2DM cases were segregated into 3 groups based on HbA1c levels. Group I-HbA1c<5 (No diabetes), Group II- HbA1c= 5-7 (Long standing controlled diabetes), Group III HbA1c >7 (Uncontrolled diabetes). Most of the patients 15(62.5%) enrolled in the study with uncontrolled diabetes and were found to be in group III (HbA1c>7). Patients with Group II (HbA1c=5-7) and Group I (HbA1c<5) were found to be 29.2% and 8.3% respectively (Table 2). Hemoglobin (g/dl) in CRF with T2DM and healthy controls were 9.6±1.6 and 13.1±2.6 respectively. Blood urea(mg/dl) and serum creatinine(mg/dl) of the CRF with T2DM and Healthy subjects were found to be 124±54, 8.5±3.4 and 38±42, 1.1±0.4 respectively (Table 3). There was a statistically significant difference between CRF with T2DM and healthy patients (p<0.001). Dental lesions in CRF with T2DM and healthy controls in dental caries, stains and calculus, gingivitis and periodontitis were 2(8%), 10(42%), 8(33%), 4(17%) and 4(15%), 14(52%), 5(19%), 4(15%) respectively (Figure 1). Oral manifestations and lesions in CRF with T2DM and healthy controls were, Uremic factor 5(21%) and 3(11%), Xerostomia 3(13%) and 10(37%), Halitosis 4(17%) and 8(30%), Pale mucosa 4(17%) and 2(7%), Glossitis 1(4%) and 1(4%), gingival enlargement 1(4%) and 1(4%) respectively (Figure 2). Ulceration, Oral pigmentations, fissured tongue accounted to 1% of cases in CRF with T2DM cases in comparison to healthy controls. Candidal infection were found to be 4(17%) in CRF with T2DM and 2(7%) in healthy individuals. The difference between the group were found to be statistically significant (P<0.005).
Table 1
Patients demographics in CRF with T2DM patients and healthy controls
|
Particulars |
Male (mean ±SD) |
Female (mean ±SD) |
Total |
|
Number of Patients(n) |
28 |
23 |
51 |
|
Mean Age of the patients |
52.1±8.8 |
48.6±5.3 |
50.4±6.3 |
|
Average duration of diabetes |
15.2±6.4 |
13.6±2.5 |
14.4±2.4 |
Table 2
Diabetic profile in CRF with T2DM patients and healthy controls
|
Diabetic Profile |
CRF with T2DM |
Healthy Controls |
||
|
|
n=24 |
% |
n=27 |
% |
|
HbA1c < 5 |
2 |
8.3 |
24 |
88.9 |
|
HbA1c 5-7 |
7 |
29.2 |
3 |
11.1 |
|
HbA1c > 7 |
15 |
62.5 |
0 |
0.0 |
|
Total |
24 |
100 |
27 |
100 |
Discussion
Oral lesions representing chronic kidney disease (CKD) is 97% worldwide. In some reports,2 prevalence of oral lesions in CKD was 100%. Oral lesions are usually due to restricted diets, malnutrition, mouth neglect, immunosuppression and the effects of medications of uremic toxins on the oral tissues.5 CKD patients on hemodialysis have also been found to be associated with reduced dental visits which further worsen the oral care.9 A wide range of oral signs, symptoms, and lesions have been reported in patients of CRF with T2DM undergoing dialysis.
In this study of 51 subjects (24 patients of CRF with T2DM and 27 healthy individuals)were aged between 30-70years with the mean age group of the male and female patients were 52.1±8.8 and 48.6±5.3 respectively. Similar studies were conducted by Bayraktar et al10 and Agarwal and Srivastava.11 The average duration of diabetes of the male patients were 15.2 ±6.4 years and the female patients were 13.6±2.5 years. Our findings were in consistent with findings of Dande R et al (2018).12 Hemoglobin (g/dl), blood urea and serum creatinine in CRF with T2DM and healthy controls were 9.6±1.6 and 13.1±2.6, 124±54, 8.5±3.4 and 38±42, 1.1±0.4 respectively. Our findings were in concordance with findings of Oyetala et al.13
Dental lesions in CRF with T2DM and healthy controls in dental caries, stains and calculus, gingivitis and periodontitis were 2(8%), 10(42%), 8(33%), 4(17%) and 4(15%), 14(52%), 5(19%), 4(15%) respectively. Gingival inflammation has been reported to be due to plaque accumulation and poor oral hygiene as reported by Olivas-escarcega et al.14 Attention has been given to general medical care, prolonged hospitalization, and hypo plastic teeth as causes of high plaque scores in these patients, as reported by Aixao et al.15 However, the frequency of gingival inflammation is low as reported by Gupta et al16 because the immunosuppression and uremia associated with renal disease alter the inflammatory response to bacterial plaques in gingival tissue. Nunn.CL et al.17 Calculus has a significant effect on gingival and periodontal disease incidence. Children with CRD exhibited an elevated level of calculus Elevated salivary pH, decreased salivary magnesium, and high levels of salivary urea and phosphorus lead to precipitation of calcium-phosphorus and calcium oxalate, and, thus, dental calculus formation as reported by Elias-Boneta et al.18 Calculus is more prevalent on the lingual surface of the lower incisors due to their proximity to the submandibular gland orifices as reported by Davidovich et al.4
Our study revealed oral manifestations and lesions in CRF with T2DM and healthy controls were, Uremic factor 5(21%) and 3(11%), Xerostomia 3(13%) and 10(37%), Halitosis 4(17%) and 8(30%), Pale mucosa 4(17%) and 2(7%), Glossitis 1(4%) and 1(4%), gingival enlargement 1(4%) and 1(4%) respectively (Figure 2). Candidal infection were found to be 4(17%) in CRF with T2DM and 2(7%) in healthy individuals. The difference between the group were found to be statistically significant (P<0.005). Our findings were in agreement with other studies as reported by Klassen and Krasko et al and Practo et al.14, 15 A common oral symptom of CRF is the sensation of a dry mouth(xerostomia), which may be caused by restricted fluid intake (necessary to accommodate the reduced excretory capacity of the kidney), adverse effects of drug therapy, and the low salivary flow rate Klassen and krasko, Proctor et al.5, 19 Patients also suffer from odorous breath (uremic breath) and sensations of metallic tastes in the mouth (uremic fetor). Uremic fetor occurs as a result of a high salivary concentration of urea, which is converted to ammonia as reported by De la Rosa-García E et al.20 Reduced erythropoietin and the resultant anemia lead to pallor of the oral mucosa. Platelet aggregation is altered during uremia as reported by Skorecki et al.21 This situation, combined with the use of heparin and other anticoagulants in hemodialysis, leads patients to become predisposed to ecchymosis, petechiae, and hemorrhages in the oral cavity as reported by Seraj et al.22 Stomatitis, mucositis, and glossitis can cause pain and inflammation of the tongue and oral mucosa. Altered taste sensations, dysgeusia, as well as bacterial and candidiasis infections can develop due to the underlying renal disease as reported by Thomas C.23 Candidiasis is seen as patients lose the ability to fight infections. Candidiasis is more frequent in transplant and on hemodialysis patients because of generalized immunosuppression.5, 14
Conclusion
This study shows increase in prevalence of oral and dental manifestations in patients of Chronic renal failure with type 2 diabetes patients than healthy controls. Gingivitis, periodontitis, and candidiasis are some of the oral lesions seen commonly in CRF with T2DM patients. As cases continues to rise early diagnosis of oral manifestations and their appropriate management can improve the quality of life of the patients.
Acknowledgement
I, would like thank the Professor and Head K. Karpagaselvi and staff members of department of oral pathology and microbiology of Vydehi Institute of Dental sciences, Bangalore for their support and guidance. I, also thank Prof Hareesa babu and Dr Girish of Department of Nephrology, Vydehi institute of medical sciences for their suggestions during the study.