- Visibility 22 Views
- Downloads 4 Downloads
- DOI 10.18231/j.jooo.2023.027
-
CrossMark
- Citation
VELscope: The challenge for the detection of orally potentially malignant lesions
Introduction
Oral cancer is the sixth most common form of cancer in the world. It represents more than 90% of all malignant neoplasms of the mouth. It affects more often from fifty years of age, and males more often than female, in a ratio of about 2:1. The main risk factors are smoking and alcohol abuse.[1]
It is really invasive and debilitating, representing for 3% of all malignant neoplasms in men and 2% of malignant neoplasms in women. This has been a rising trend for women in the last 30 years, and it is persisting now for young people.[1]
Bad oral hygiene, poorly fitted dental prosthesis, vitamin deficiency, and the papilloma virus are all confound factors in addition to smoking and alcohol usage.[2] Unfortunately, only 35% of the malignant lesions are detected in the early stages due to the fact that these lesions start at the basal cell layer and cannot be seen by the naked eye.[3], [4] In addition, there is a lack of information about this disease, and protection is still inadequate.[5]
The Oral Cancer Prevention Program should advocate for a comprehensive and standardized examination that includes medical records, habits (tobacco and alcohol), clinical examination (Extraoral and Intraoral), and lesion inspection.[6], [7]
Oral cancer screening and early identification in high-risk populations has been recommend as a way to reduce morbidity and mortality.[8]
Visual detection of premalignant oral lesions, on the other hand, has remained a difficulty all over the world. One explanation for this is that early oral cancer and premalignant lesions are generally small and lack the clinical features seen in advanced cases: ulceration, induration, discomfort, or lymphadenopathy of the cervical region.[9]
As well as their clinical subtlety, premalignant lesions are highly heterogeneous in their appearance and may mimic a variety of benign or reactive conditions.[10] Furthermore, it is becoming increasingly clear that some premalignant and early carcinogenic lesions are not visible to the human eye. As a result, more oral cancer screening tools are desperately need.[11]
In recent years, luminous detection systems (chemiluminescence and tissue autofluorescence techniques) have been add to visual tools for assisting in the diagnosis of oral cancer, with the goal of improving detection and increasing our capacity to identify potentially malignant lesions, which are lesions that exhibit a change in shape or color on clinical or histological appearance.[12]
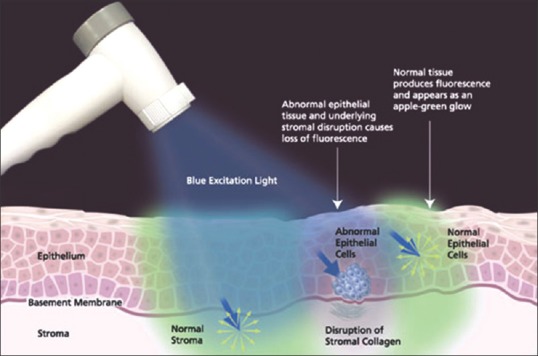
Chemiluminescence and auto fluorescent imaging, work on the assumption that neoplastic and pre-neoplastic tissues that have undergone abnormal metabolic or structural changes have different absorbance and reflectance properties when exposed to specific wavelengths of light.
In the last decade, light-based technology has been adapted and marketed for use in the oral cavity (chemiluminescence: ViziLite; autofluorescence: VELscope (Visual Enhanced Light scope).[13]
Tissue autofluorescence has been used to detect premalignant and early cancers of the lung, uterine cervix, skin, and, more recently, the oral cavity. It was discover about 30 years ago that tissue fluorescence might be utilized for cancer detection.[14], [15]
VELscope (Visually enhanced lesion scope)
Simple hand-held device manufactured by LED Dental Inc., Vancouver based company, BC, Canada. It was developed by British Columbia Cancer Agency in collaboration with MD Anderson Cancer Center, became commercially available after FDA approval in 2006.[16]
It used to identify changes in oral mucosal tissues by observing the fluorescence of oral tissues in response to light excitation.
This system detects the loss of fluorescence in visible and not visible high-risk lesions using a handpiece emitting light at (400-460 nm) wavelength range. Under this light, the normal mucosa emits green color fluorescence, while the abnormal area absorbs the fluorescent light and dark patches appear.[7]
Case reports about the use of VELscope on referred or review patients at specialist oral dysplasia clinics in British Columbia, Canada, comprised the early research supporting its application. They discovered that VELscope helped uncover dysplastic and malignant lesions that were not evident by conventional oral examination and raised suspicion of lesions that would not have been subject to biopsy otherwise. In one example, there was widespread erythema; The VELscope identified a region that turned out to be a well-differentiated carcinoma later on. It was also useful in defining the borders of existing tumors if the malignant tissue spread beyond what was clinically evident. While the VELscope was only used in specialized settings, these case reports provided the first indication that the instrument could help clinicians distinguish between dysplasia and normal oral mucosa.[17], [4]
This device recognized by the World Health Organization in 2009 as a commercialized medical device that addresses global health concerns and is accessible to low and middle.
VELscope is intended to use by dentists or health-care providers as an adjunct to traditional oral examination by incandescent light to enhance the visualization of oral income countries.
Supported by clinical studies illustrating the efficacy of the VELscope’s tissue fluorescence visualization, more than 25 million VELscope examinations have performed by over 15,000 dental practitioners in 23 countries worldwidemucosal abnormalities. It's also designed to help surgeons identify abnormal tissue around a clinically apparent lesion and, as a result, determine the proper margin for surgical excision.[11]
VELscope causes fluorescence excitation of specific chemicals in tissues by using visible light with a wavelength of 430 nm. When used in conjunction with a well-thought-out clinical assessment process that considers the patient's age as well as risk factors such as tobacco, alcohol, and immunological status, the VELscope improves the clinician's ability to detect oral changes that could indicate pre-malignant or malignant cellular transformation.
Lesions that are VELscope-positive and absorb light need to be followed with caution and if they do not resolve within a 2-week period, then further assessment and biopsy are generally advised. It is much better to occasionally sample tissue that turns out to be benign than to fail to diagnose dysplastic or malignant lesions. In our fight to protect patients from cancer, the VELscope improves our odds for early detection, hopefully resulting in fewer deaths from oral cancer.[17]
Uses of VELscope
Several studies have investigated the effectiveness of the VELscope system as an adjunct to visual examination for:
Improving the distinction between normal and abnormal tissues (both benign and malignant changes).[18]
Differentiating between benign and dysplastic/malignant changes.
Identifying dysplastic/malignant lesions that are visible to naked eye under white light.[19]
Surgeon can use the VELscope to determining the appropriate margin for surgical excision.[20]
Component of VELscope
It comprises of a bench top case with a 120 W metal halide arc lamp, as well as a system of filters and reflectors tuned for producing near-ultraviolet/blue light between 400 and 460 nm and a portable device for direct observation.
A camera can be link to the hand piece for documentation purposes if necessary. Wide field autofluorescence photos can be digitally process to indicate worrisome zones in real time. The autofluorescence seen in wide-field pictures of normal oral mucosa is mostly cause by stromal collagen.
The loss of stromal autofluorescence is relate to oral neoplasia. Inflammation and other benign lesions are link to a loss of stromal autofluorescence, which can compromise diagnostic specificity, especially in the low-risk group. [21]
Technique of autofluorescence visualization
In 1924, the autofluorescence of tissue and its potential application in cancer detection were first described (Policard, 1924). When excited with light between 375 and 440nm, naturally occurring fluorochromes (e.g. collagen, elastin, keratin, FAD, NADH) located in the epithelial cell lining and submucosa of the oral cavity show fluorescence in the green spectral range, which is define as Fluorescence visualization retained (Richards-Kortum & Sevick-Muraca, 1996). (FVR). [22]
Because of the disruption in the distribution of these fluorochromes, malignant or dysplastic changes induce full loss of normal tissue fluorescence, termed as Fluorescence visibility loss (FVL).[21], [15] Autofluorescence spectroscopy, according to the literature, offers a sensitivity and specificity of more than 95% for distinguishing malignant tumors from healthy oral tissue.
Autofluorescence imaging to conventional clinical examination could possibly improve sensitivity and specific.[22], [23]
The VELscope's inability to distinguish high-risk lesions from low-risk lesions (Awan et al., 2011) and its high rate of false-positive results have been questioned in recent investigations.[24]
VELscope generations
The first-generation VELscope®, which was released in 2006, uses direct tissue autofluorescence to highlight oral mucosal abnormalities. A blue light is used to observe intraoral locations with this basic device. Normal tissues fluoresce brilliant green under the blue light, but diseased tissue appears black. However, this generation's blue light output was weak, necessitating complete darkness in the operatory for proper visualization.[25]

The second-generation device was develope after two years and had significantly better blue light output than first generation.[20]

The last and device is (VELscope Vx) was develope in 2010. Vx system is equivalent to the earlier generation VELscope system. Although changes have been made with respect to the originally cleared VELscope system to integrate the light source into the Handpiece and to allow cordless operation by means of a rechargeable battery. The theory of operation, underlying mechanisms of action and key performance specifications, are unchanged.[24]
Advantages
The big advantage is that it is a non-traumatic technique used by dentists for the detection of pre-malignant and malignant lesions in early stages, one of the effective approaches for improving treatment effectiveness, boosting survival rates, and maintaining a high quality of life is early identification.[26]
The recurrence rate ranges from 40 to 50% after 5 years of treatment. But when the disease is detected early, the percentage of recurrence is reduced to 10–20%.[27]
Study showed that the VELscope was useful in confirming the presence of oral leukoplakia and erythroplakia and other oral mucosal disorders.[20]
Clinical detection of oral cancer, gold standard are diagnostic biopsies, by using a VELscope we try to pick up the most favorable site for biopsy considering economic benefits and decreasing overall rate of number of biopsies.[28]
They could be a simple and low-cost method of determining margins.[29]
Quick, painless and highly effective examination.[30]
It is a simple hand-held fluorescence visualization tool for the direct visualization of tissue fluorescence and easy to use.[21]
Disadvantages
The principal weakness of light-based detection systems are their low specificity.
The fact that there is no evidence to support their cost effectiveness in comparison with COE.
The uncertainty of whether the application of the test has reduced mortality.[31]
The practitioners require more training and experience with the device as well as in mucosal pathology.[32], [33]
Any positive findings require reassessment to limit over-diagnosis.[33]
Low sensitivity.[8]
The false negative results are very high so there is feeling of insecurity for clinician and patient.[34]
Psychological trauma for those with false negative results.
Only adjuvant.[8]
Studies
Using the VELscope device, autofluorescence imaging is a non-invasive and quick method of evaluating the oral mucosa and diagnosing oral cavity abnormalities. Given the technique's potential benefits, it's critical to determine whether it can be used for screening, which is why we've conducted a review of studies on autofluorescence (VELscope). For each research, the following formulas were used to calculate sensitivity and specificity values:
Sensitivity = [true positives/ (true positive + false negative)] ×100
Specificity = [true negatives/ (true negative + false positives)] ×100
1st study
The local ethics committee at the University Medical Centre in Hamburg, Germany, gave their approval to the study (2011). The institutional cancer board examined and approved the clinical protocol before enrolling study participants. Each patient provided written informed consent prior to the start of the trial.
120 patients with suspected oral pre-malignant lesions were split into two groups at random. A traditional white light examination was perform on the first group of 60 patients. In addition to the white-light examination, the other 60 patients were evaluate with an autofluorescence visualization instrument called VELscope.
Biopsies were obtained from all patients in both examination procedures.
Results
In the first group, 45 patients were found to be positive after being test with white light. A dysplastic or pre-malignant lesion was find in 41 of the samples. In the second group 55 patient were diagnosed positive. Here the biopsies revealed that 47 patients had a pre-malignant lesion. Remaining 5 patients were diagnosed negative, whereas 1 patient had a dysplastic lesion and 4 patients showed no findings. Based on these results the sensitivity, specificity and confidence intervals were calculated. The sensitivity for group 1 is 75.9% and the specificity is 33.3%. The sensitivity for group 2 is 97.9% and the specificity is 41.7%.[35]
2nd study
Michaell A. Huber, University of Texas Health Science Center at San Antonio, USA. In 2009 year examined 130 patients.
Inclusion criteria included males and females over 18 years of age all of them are smoked and concentrated on heavy smokers' patient who at least smoked one packet of cigarettes per day.
Results
All of the patient are examining by two ways (COE + VELscope) comparing clinical findings received through traditional examination with those obtained using VELscope While conventional methods identified ten suspicious tumors that required monitoring or biopsy, VELscope discovered none, which raises concerns about its usage for screening purposes.[36]
3rd study
The aim of this study was to determine the condition of oral soft tissues in old age patients and the impact of oral health on their quality of life because precancerous lesions and oral carcinoma are more common in the elderly compared to the younger population.
Almost 90% of oral cancers occur in patients older than 50 years so that early detection of oral mucosal diseases in elderly and because of the high rate of malignant transformation, potentially malignant conditions necessitate a thorough investigation. The study was perform in the University Dental Clinic center in Skopje, NM in 2019 for 300 patients over 60 years old. Clinical intra and extraoral observation and VELscope mucosal tissue examination was done.
Result
Tissue changes were classified as inflammatory, traumatic, dysplastic and other. Abnormal tissue was associated with autofluorescence loss and dark appearance in contrast to the surrounding healthy tissue. In 21% of patient's abnormal premalignant lesions were detected. Leukoplakia was the most common pre-malignant disorder 42 (12. 6%), 16 (4. 8%) had lichen planus, 6 (1. 8%) actinic cheilitis and 5 patients (1. 5%) were diagnosed with squamous cell carcinoma. Also, they found 118, 38,54 patients diagnosed as inflammatory, traumatic, infectious changes respectively so, the study conclude that the VELscope fluorescence instrument can be used as a part of diagnostic process to detect abnormal tissue and oral lesions that might have been overlooked.[37]
4th study
Fifty patients (32 males and 18 females) with oral cavity or lip cancer history treated in the Department of Maxillofacial Surgery at Rydygier’s Hospital in (Cracow, Poland) were enrolled in this study. Investigation of oral mucosa condition involved conventional clinical visual examination and autofluorescence examination. All detected oral lesions (only in conventional or autofluorescence examination and in both), that had not responded to the conservative therapy after 14 days, were biopsied.
Result
Thirteen pathological lesions were detect in ten patients. Nine patients had single lesion, whereas one had multiple ones.
Florescence visualization loss was observed in eleven of twelve (91.7%) clinically diagnosed pathological lesions. In autofluorescence examination, there was one area of FVL detected, that was not visible in incandescent light source.
Two lesions were totally cure after 14-days conservative therapy. Eleven lesions were biopsied. Oral epithelial dysplasia was confirm in three lesions (27.3%). Due to complete loss of fluorescence within two lesions, they were biopsied again, using VELscope to choose the precise biopsy side. The histopathological assessment confirmed carcinoma in situ and invasive carcinoma.
Autofluorescence examination showed a sensitivity of 100%, as all high – risk oral lesions showed FVL. However, the autofluorescence was not highly specific for Dysplasias and cancers, as FVL was observed in 7 (87.5%) of the benign oral lesions, leading to a low specificity of 12.5%.[20] ([Table 1])
|
Authors |
Year |
VELscope investigations |
Oral Pathology |
No. of samples |
Result |
|
(Rana et al.,) [38] |
2012 |
Autofluorescence examination vs. white light examination |
OPMD |
289 |
VELscope is a useful new diagnostic device for the detection of oral cancer diseases. |
|
(Hanken et al.) [35] |
2013 |
Early detection with VELscope |
OPMD |
120 |
VELscope® is a simple noninvasive way to find OPMD. |
|
(Rashid et al.)[5] |
2014 |
Chemiluminescence vs. tissue autofluorescence in detection of OPMD |
OPMD |
25 |
VELscope® may detect erythematous lesions or benign inflammations as a false positive. |
|
(Jane-Salas et al.)[32] |
2015 |
Conventional oral examinassions vs. Autofluorescence technique VELscope |
Oral lesions |
60 |
No clinical benefits were obtained using the VELscope system. |
|
(Ohnishi et al.,)[39] |
2016 |
Tissue fluorescence examination VELscope |
Carcinoma in situ |
17 |
Fluorescence examination could represent a simple, cost-effective screening. |
|
(Burian et al.,)[40] |
2017 |
Tissue fluorescence examination VELscope |
Oral soft tissue lesions or carcinoma in situ |
90 |
VELscope® could help clinicians and help to define biopsy margins. |
|
(Farah et al.)[41] |
2018 |
Differences between white light and autofluorescence on oral potentially malignant disorders (OPMD) detected margins. |
Oral epithelial dysplasia, oral lichen planus, oral lichenoid dysplasia |
11 |
Autofluorescence determined margins are safer. |
Discussion
In the pathological clinical field, the use of novel diagnostic tools, particularly noninvasive ones, can be a significant boon. Oral malignant lesions account for a significant portion of all cancerous lesions. As a result, having a reliable, quick, and exact diagnostic tool can be beneficial to a clinician who deals with a wide range of patients on a routine basis.
According to available evidence, VELscope can help detect malignant lesions, with sensitivity and specificity values ranging from 18.4 percent to 98 percent and 81 percent to 100 percent, respectively.[20] Despite the wide range, several studies have found that VELscope can assist detect dysplastic lesions that are missed by traditional oral exams; for these reasons, VELscope looks to be a valuable tool in monitoring patients with a history of head and neck cancer.[41], [18]
According to some studies, the device can distinguish normal mucosa from severe dysplasia/carcinoma in situ (CIS) or invasive cancer with a sensitivity of 98 percent and a specificity of 100 percent.[21]
The VELscope, according to (Kois and Truelove, 2006) can help with patient assessment since it improves the clinician's capacity to detect oral alterations that could indicate pre-malignant or malignant cellular transformation.[17]
In the presence of highly inflamed lesions, false positive findings are possible, and using the scope alone may result in failure to detect regions of dysplasia, but the authors' experience has been that to use the VELscope improves clinical decision-making about the nature of oral lesions and aids in biopsy decisions. The use of the VELscope has allowed practitioners to determine the appropriate place for biopsy when tissue changes are widespread or encompass large portions of the mouth.
No one technique or process, as with other clinical diagnostic activities; is sufficient, and all physicians are recommended to assess patients and recall and biopsy lesions that do not clear within a predetermined time range using appropriate clinical practice. It is yet unknown whether using the VELscope would enhance early detection and lead to fewer mouth cancer mortality.[17]
According to (Yamamoto et al., 2017) for diagnosis, VELscope or visual fluorescence evaluations cannot replace histology. They could, however, be a simple and low-cost margin determination method that adds the sensitivity of a traditional oral examination.
Ganga et al., 2017 VELscope was use to compare the differences between a conventional oral examination (COE) and an autofluorescence examination. The results of the VELscope were compare to histological findings. The authors claim that VELscope alone cannot be use as a diagnosis tool since it produces a large proportion of false positives. It could be use to help patients with mucosal lesions feel less anxious.
Mehrotra et al., 2010 argued that since not all dysplastic lesions displayed loss autofluorescence (LAF), its use in routine practice should be discouraged as it can result in missed lesions and a false sense of security. Of concern, VELscope has a high rate of false positives, with reported specificities ranging between (15 to 81%). This suggests that VELscope is a poor differentiator between benign and dysplastic lesions. In particular, inflammatory lesions typically display LAF as well and, thus, act as confounders when using VELscope. As the majority of oral mucosal lesions seen in general practice are benign in nature, incorrect interpretation can lead to overestimation of oral mucosal abnormalities and patient harm through unnecessary referrals and biopsies.[34]
Poh et al., 2006 direct tissue fluorescence imaging has been shown to improve the identification of malignant margins. In some cases, the loss of fluorescence was extend beyond 25 mm from the clinically visible margins of the lesion. This is particularly intriguing because one of the most difficult and contentious topics in the treatment of oral squamous cell carcinoma is determining how much of the surrounding normal-looking tissues must be removed in addition to the tumor mass. In order to eliminate any clinically occult high-risk areas, surgeons typically extend 10 mm or more beyond the margins of a malignant lesion. So, the possibility of using tissue fluorescence as a guide for detecting field modifications and tumor border extension during surgical excision is quite intriguing, but more research is needed to confirm this concept.[42]
Conclusion
Detection of oral potential malignant lesions before they advance to oral squamous cell carcinoma is necessary to improve survival rates for oral cancer. Evidence indicates that COE is a poor discriminator of oral mucosal lesions and this has led to the development of several adjunctive visualization aids.
The VELscope tool is a non-invasive oral mucosa test that can assist an expert physician in locating oral pre-malignant lesions and the proper place for biopsies within the altered mucosa. Nonetheless, because of the issue of false positive results, the data should be regarded with caution. The device should not be utilized by untrained practitioners, and it cannot be used as a substitute for the gold standard of any histological examination. The tool can only be recommended at this time to rule out any suspicious lesions.
Source of Funding
None.
Conflict of Interests
There is no conflict of interests to declare.
Authors’ Contributions
All authors equally contributed to this project and manuscript. All authors read and approved the final manuscript.
References
- C Porcheri, CT Meisel, T Mitsiadis. Multifactorial contribution of notch signaling in head and neck squamous cell carcinoma. Int J Mol Sci 2019. [Google Scholar] [Crossref]
- A Stornetta, V Guidolin, S Balbo. Alcohol-derived acetaldehyde exposure in the oral cavity. Cancers (Basel) 2018. [Google Scholar] [Crossref]
- AK Chaturvedi, WF Anderson, J Lortet-Tieulent, MP Curado, J Ferlay, S Franceschi. Worldwide trends in incidence rates for oral cavity and oropharyngeal cancers. J Clin Oncol 2013. [Google Scholar]
- CF Poh, SP Ng, PM Williams, L Zhang, DM Laronde, P Lane. Direct fluorescence visualization of clinically occult high-risk oral premalignant disease using a simple hand-held device. Head Neck 2007. [Google Scholar]
- R Shashidara, HS Sreeshyla, US Sudheendra. Chemiluminescence: A diagnostic adjunct in oral precancer and cancer: A review. J Cancer Res Ther 2014. [Google Scholar]
- MD Mignogna, S Fedele. Oral cancer screening: 5 minutes to save a life. Lancet 2005. [Google Scholar]
- A Trullenque-Eriksson, M Muñoz-Corcuera, J Campo-Trapero, J Cano-Sánchez, A Bascones-Martínez. Analysis of new diagnostic methods in suspicious lesions of the oral mucosa. Med Oral Patol Oral Cir Bucal 2009. [Google Scholar]
- MW Lingen, JR Kalmar, T Karrison, PM Speight. Critical evaluation of diagnostic aids for the detection of oral cancer. Oral Oncol 2008. [Google Scholar]
- C Scully, JV Bagan, C Hopper, JB Epstein. Oral cancer: current and future diagnostic techniques. Am J Dent 2008. [Google Scholar]
- S Fedele. Diagnostic aids in the screening of oral cancer. Head Neck Oncol 2009. [Google Scholar] [Crossref]
- LL Patton, JB Epstein, AR Kerr. Adjunctive techniques for oral cancer examination and lesion diagnosis: a systematic review of the literature. J Am Dent Assoc 2008. [Google Scholar]
- K Matsumoto. Detection of potentially malignant and malignant lesions of oral cavity using autofluorescence visualization device. Kokubyo Gakkai Zasshi 2011. [Google Scholar]
- G Lodi, C Scully, M Carrozzo, M Griffiths, PB Sugerman, K Thongprasom. Current controversies in oral lichen planus: report of an international consensus meeting. Part 2. Clinical management and malignant transformation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005. [Google Scholar]
- I Pavlova, M Williams, A El-Naggar, R Richards-Kortum, A Gillenwater. Understanding the biological basis of autofluorescence imaging for oral cancer detection: high-resolution fluorescence microscopy in viable tissue. Clin Cancer Res 2008. [Google Scholar]
- E Svistun, R Alizadeh-Naderi, A El-Naggar, R Jacob, A Gillenwater, R Richards-Kortum. Vision enhancement system for detection of oral cavity neoplasia based on autofluorescence. Head Neck 2004. [Google Scholar]
- HM Ayoub, TL Newcomb, GB Mccombs, M Bonnie. The Use of Fluorescence Technology versus Visual and Tactile Examination in the Detection of Oral Lesions: A Pilot Study. J Dent Hyg 2015. [Google Scholar]
- JC Kois, E Truelove. Detecting oral cancer: a new technique and case reports. Dent Today 2006. [Google Scholar]
- HZ Marzouki, TTV Vu, R Ywakim, P Chauvin, J Hanley, KM Kost. Use of fluorescent light in detecting malignant and premalignant lesions in the oral cavity: a prospective, single-blind study. J Otolaryngol Head Neck Surg 2012. [Google Scholar]
- KK Mcnamara, BD Martin, EW Evans, JR Kalmar. The role of direct visual fluorescent examination (VELscope) in routine screening for potentially malignant oral mucosal lesions. Oral Surg Oral Med Oral Pathol Oral Radiol 2012. [Google Scholar]
- KH Awan, PR Morgan, S Warnakulasuriya. Evaluation of an autofluorescence based imaging system (VELscopeTM) in the detection of oral potentially malignant disorders and benign keratoses. Oral Oncol 2011. [Google Scholar]
- PM Lane, T Gilhuly, PD Whitehead, H Zeng, C Poh, S Ng. Simple device for the direct visualization of oral-cavity tissue fluorescence. J Biomed Opt 2006. [Google Scholar] [Crossref]
- CS Betz, H Stepp, P Janda, S Arbogast, G Grevers, R Baumgartner. A comparative study of normal inspection, autofluorescence and 5-ALA-induced PPIX fluorescence for oral cancer diagnosis. Int J Cancer 2002. [Google Scholar]
- B Kulapaditharom, V Boonkitticharoen. Performance characteristics of fluorescence endoscope in detection of head and neck cancers. Ann Otol Rhinol Laryngol 2001. [Google Scholar]
- B Balevi. Evidence-based decision making: should the general dentist adopt the use of the VELscope for routine screening for oral cancer?. J Can Dent Assoc 2007. [Google Scholar]
- N Bhatia, Y Lalla, AN Vu, CS Farah. Advances in optical adjunctive AIDS for visualisation and detection of oral malignant and potentially malignant lesions. Int J Dent 2013. [Google Scholar] [Crossref]
- A Meena, SK Satoskar. Early Detection of Oral Pre-Cancerous Lesions: Recent Advances. Int J Med Public Health 2012. [Google Scholar]
- LAG Ries, D Melbert, M Krapcho, DG Stinchcomb, N Howlader, MJ Horner. SEER Cancer Statistics Review, 1975-2005. . [Google Scholar]
- WL Curvers, R Singh, MB Wallace, LMWK Song, K Ragunath, HC Wolfsen. Identification of predictive factors for early neoplasia in Barrett's esophagus after autofluorescence imaging: a stepwise multicenter structured assessment. Gastrointest Endosc 2009. [Google Scholar]
- S Cânjău, DCM Todea, C Sinescu, MO Pricop, VF Duma. Fluorescence influence on screening decisions for oral malignant lesions. Rom J Morphol Embryol 2018. [Google Scholar]
- C Paderni, D Compilato, F Carinci, G Nardi, V Rodolico, LL Muzio. Direct visualization of oral-cavity tissue fluorescence as novel aid for early oral cancer diagnosis and potentially malignant disorders monitoring. Int J Immunopathol Pharmacol 2011. [Google Scholar]
- B Balevi. Assessing the usefulness of three adjunctive diagnostic devices for oral cancer screening: a probabilistic approach. Community Dent Oral Epidemiol 2011. [Google Scholar]
- E Jané-Salas, A Blanco-Carrión, L Jover-Armengol, J López-López. Autofluorescence and diagnostic accuracy of lesions of oral mucosa: a pilot study. Braz Dent J 2015. [Google Scholar]
- DM Laronde, CF Poh, PM Williams, TG Hislop, L Zhang, C MacAulay. A magic wand for the community dental office? Observations from the British Columbia Oral Cancer Prevention Program. J Can Dent Assoc 2007. [Google Scholar]
- R Mehrotra, M Singh, S Thomas, P Nair, S Pandya, NS Nigam. A cross-sectional study evaluating chemiluminescence and autofluorescence in the detection of clinically innocuous precancerous and cancerous oral lesions. J Am Dent Assoc 2010. [Google Scholar]
- H Hanken, J Kraatz, R Smeets, M Heiland, M Blessmann, W Eichhorn. The detection of oral pre-malignant lesions with an autofluorescence based imaging system (VELscope TM)-a single blinded clinical evaluation. Head Face Med 2013. [Google Scholar]
- MA Huber. Assessment of the VELscope as an adjunctive examination tool. Tex Dent J 2009. [Google Scholar]
- A Mijoska, G Kovacevska, G Tomov. Oral tissue condition in prosthodontic geriatric patients. Knowl Intl J 2019. [Google Scholar]
- E Burian, C Schulz, F Probst, B Palla, M Tröltzsch, F Maglitto. Fluorescence based characterization of early oral squamous cell carcinoma using the Visually Enhanced Light Scope technique. J Craniomaxillofac Surg 2017. [Google Scholar]
- Y Ohnishi, T Fujii, Y Ugaki, H Yasui, M Watanabe, S Dateoka. Usefulness of a fluorescence visualization system for the detection of oral precancerous and early cancerous lesions. Oncol Rep 2016. [Google Scholar]
- CS Farah, L Mcintosh, A Georgiou, MJ Mccullough. Efficacy of tissue autofluorescence imaging (VELScope) in the visualization of oral mucosal lesions. Head Neck 2012. [Google Scholar]
- M Rana, A Zapf, M Kuehle, NC Gellrich, AM Eckardt. Clinical evaluation of an autofluorescence diagnostic device for oral cancer detection: a prospective randomized diagnostic study. Eur J Cancer Prev 2012. [Google Scholar]
- Y Wang, K Fang, S Jung, J Zheng, S Hao. Excisional biopsy with margin control for oral cancers. Head Neck 2010. [Google Scholar]
