- Visibility 131 Views
- Downloads 20 Downloads
- DOI 10.18231/j.jooo.2024.041
-
CrossMark
- Citation
Mulberry lesion: Fibro-epithelial hyperplasia with an unusual clinical presentation
Introduction
Hyperplasia is defined as an abnormal increase in tissue due to any irritant or trauma which is not neoplastic but cause aesthetic as well as functional problems. Hyperplastic lesions are reactive in nature and can be seen anywhere in the oral cavity as nodular swellings most commonly seen on gingiva which are reactive in nature and can exhibit a plethora of clinical presentations[1] & presents an exuberant tissue response to a non specific irritant. It usually appears in the gingiva between two teeth, but is found also on the lip, tongue, palate and occasionally on the buccal mucosa. Predisposing factors for the occurance of these type of entities generally include chronic irritation like repeated biting, foreign bodies, calculus and ill fitting dentures. [2] We are hereby presenting a case of long standing fibro epithelial hyperplasia with its clinical presentation as well as its management.
Case Report
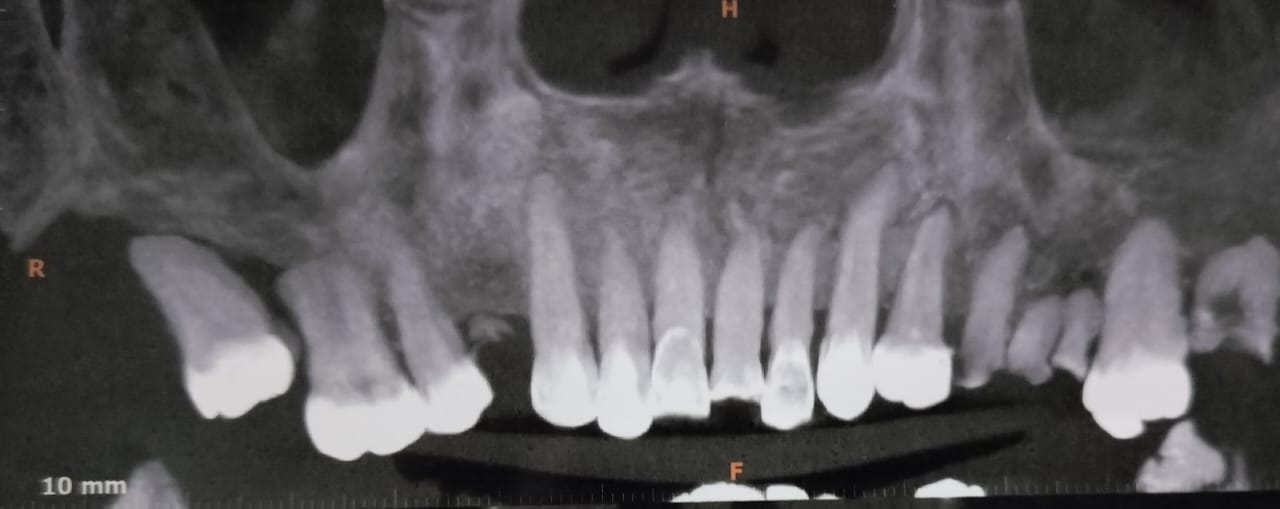
A 55 year old female reported to our department of Oral and Maxillofacial Surgery with the chief complaint of a growth inside her mouth since 3 years ([Figure 1]). Past medical and dental history was non contributory. The growth was smaller in size initially was slowly grew to its present size and was not associated with any pain. On clinical examination, a red, lobulated mulberry shaped sessile exophytic growth approximately 4cms* 3cms in size was present over hard palate region almost crossing the midline medially and extending to the hard palate – soft palate junction posteriorly ([Figure 2]). On palpation, the growth was found to be firm to soft in consistency, non tender on palpation and bleeding on probing was absent. Mobility was also present with relation to 17. Patient was then adviced for routine blood and radiological investigations. Blood investigations revealed no abnormality and all the values were under normal limits and radiologically bone loss was present around 17 region([Figure 3]).
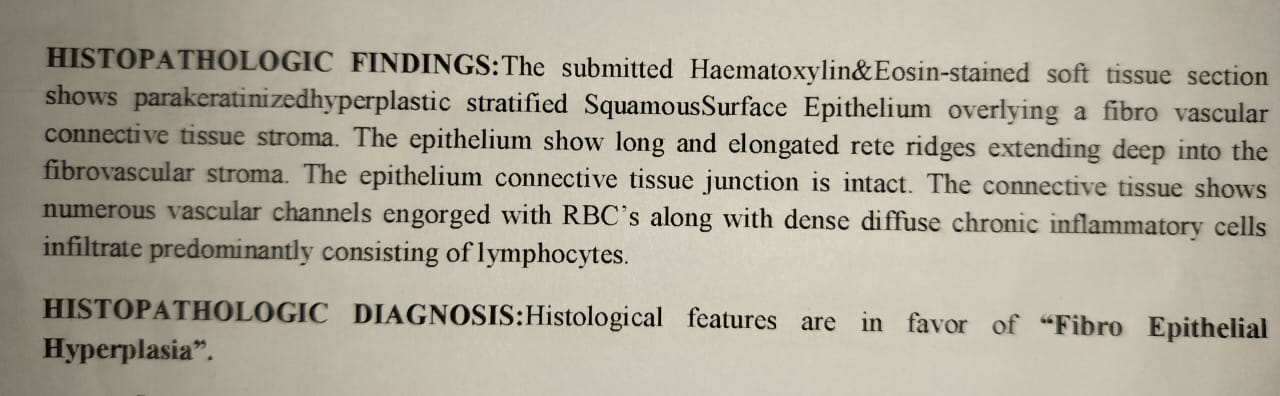
Incisional biopsy was done for the patient and the results revealed it to be a fibro epithelial hyperplasia with the histopathological description of a connective tissue with the involvement of various vascular channels as well as abundance of chronic inflammatory cells ([Figure 4]).
Excision was carried out for the lesion after the histopathological analysis under local anesthesia. Local anesthetic with vasoconstrictor was injected in the periphery of lesion to aid in vasoconstriction. The lesion was excised with a peripheral margin of 2mm along with the extraction of 17. Haemostasis was achieved by bipolar electrocautery as well as adrenaline soaked pressure dressings and suturing of the socket of 17 ([Figure 5]). Excised specimen was also sent for histpathological analysis which confirmed the initial diagnosis (fig6). Healing time was uneventful and patient is currently on regular follow ups to check for any recurrence.




Discussion
Oral cavity serves as a common stage for the performances of many soft tissue overgrowths and poses a state of confusion for the observer to diagnose through a diverse form of clinical presentations. It is constantly exposed to external and internal stimuli & shows a wide range of diseases, from developmental to reactive to inflammatory to neoplastic.[3] Although any growth which is out of the contour of the oral cavity is regarded as an overgrowth but on a bigger scale, there is usually either neoplasia or hyperplasia which is at play.
Reactive hyperplasia comprises of a group of fibrous connective tissue lesions that commonly occur in the oral mucosa as a result of injury or chronic irritation.[4] Daley et al. proposed that the word “focal fibrous hyperplasia,” which suggests a reactive tissue response, be used instead of “fibroma,” which implies a benign neoplastic proliferative fibrous connective tissue, which is wrong. It is the most prevalent oral mucosal mass in adults, accounting for roughly 1.2% of the population.[5] Chronic trauma can induce inflammation which produce granulation tissue with endothelial cells, chronic inflammatory cells and later fibroblasts which proliferates and manifest as an overgrowth.
Clinically, it is an elevated, pedunculated or sessile mass with a smooth, lobulated, or even warty surface which commonly is ulcerated and tends to bleed spontaneously or upon slight trauma. [6] Histologically hyperplasia can be presented with or without atypia as described in the classification given by WHO. In above mentioned case, the diagnosis came out to be fibro epithelial hyperplasia which is a reactive lesion and usually manifests itself as a pedunculated or a sessile overgrowth in any part of the oral cavity. Local excision with the removal of irritant is the most favourable course of treatment as it reduces the possibilities of recurrence[7] although about 16% of the cases show recurrence.[8] Since the appearance is similar to other reactive lesions as well as neoplastic lesions histopathological and radiological examination is very vital for the correct diagnosis and proper treatment planning.
Source of Funding
None.
Conflict of Interest
None.
References
- SA Torres. Inflammatory fibro-epithelial hyperplasia related to a fixed implant-supported prosthesis: A case report. J Clin Exp Dent 2018. [Google Scholar]
- B Gandhi, J Dhuvad, A Johnson, D Bhavsar. Reactive lesions of oral cavity. Natl J Integr Res Med 2018. [Google Scholar]
- B Niranjan, ND Shashikiran, A Dubey, S Singla, C Shukla, S Mali. A Rare Gingival Lesion in Children: Fibroepithelial Hyperplasia. Int J Clin Pediatr Dent 2022. [Google Scholar]
- JA Regezi, JJ Sciubba. . Oral Pathology: Clinical-Pathologic Correlation 2008. [Google Scholar]
- TD Daley, GP Wysocki, PD Wysocki. The major epulides: clinico pathological correlations. J Can Dent Assoc 1990. [Google Scholar]
- Y Kfir, A Buchner, L S Hansen. Reactive lesions of the gingiva. A clinicopathological study of 741 cases. J Periodontol 1980. [Google Scholar]
- NJ Naderi, N Eshghyar, H Esfehanian. Reactive lesions of the oral cavity: A retrospective study on 2068 cases. Dent Res J (Isfahan) 2012. [Google Scholar]
- SN Bhaskar, JR Jacoway. Peripheral fibroma and peripheral fibroma with calcification. J Am Dent Assoc 1966. [Google Scholar]
How to Cite This Article
Vancouver
Mundepi N. Mulberry lesion: Fibro-epithelial hyperplasia with an unusual clinical presentation [Internet]. J Oral Med Oral Surg Oral Pathol Oral Radiol. 2025 [cited 2025 Sep 04];10(3):214-216. Available from: https://doi.org/10.18231/j.jooo.2024.041
APA
Mundepi, N. (2025). Mulberry lesion: Fibro-epithelial hyperplasia with an unusual clinical presentation. J Oral Med Oral Surg Oral Pathol Oral Radiol, 10(3), 214-216. https://doi.org/10.18231/j.jooo.2024.041
MLA
Mundepi, Naman. "Mulberry lesion: Fibro-epithelial hyperplasia with an unusual clinical presentation." J Oral Med Oral Surg Oral Pathol Oral Radiol, vol. 10, no. 3, 2025, pp. 214-216. https://doi.org/10.18231/j.jooo.2024.041
Chicago
Mundepi, N.. "Mulberry lesion: Fibro-epithelial hyperplasia with an unusual clinical presentation." J Oral Med Oral Surg Oral Pathol Oral Radiol 10, no. 3 (2025): 214-216. https://doi.org/10.18231/j.jooo.2024.041
