Introduction
A simple bone cyst (SBC) was first described by Lucas in 1929 as traumatic bone cyst.1 The international histological classification adopted by the WHO for odontogenic tumors uses the term “solitary bone cyst.”1 The 2017 revised WHO classification of odontogenic and non-odontogenic cysts has placed this under the category of pseudocysts and used the term simple bone cyst.2 Pseudocysts are defined as pathological cavities without an epithelial lining and with clinical and radiological findings similar to those of true cysts. It is a rare non-neoplastic, non-odontogenic, intraosseous bone cyst.1, 3 It has been referred by various names which include solitary bone cyst, traumatic bone cyst, extravasation cyst, unicameral bone cyst, hemorrhagic cyst, and idiopathic bone cyst.2, 3 It commonly affects the metaphysis of long bones like the femur and humerus. SBC prevalence in maxilla and mandible is less than 1% and incidence is 1% of the jaw cyst. Almost 89% of the cases occur in mandible and 11% occur in maxilla.1, 3 This article, which reports a rare case of SBC of the mandible, is in accordance with CARE guidelines. A study in brazil showed occurrence of 2.4% cases in all jaw cystic lesions.3, 4 The aetiology of the cyst is unknown, but various proposed theories includes traumatic hemorrhagic theory, infectious theory, lesion degeneration theory, local thrombosis, developmental theory, etc.,5 out of which traumatic hemorrhagic theory is widely accepted.4, 6 According to this theory, trauma leads to intramedullary hemorrhage. Usually, the hemorrhage will form a clot but in SBC, there is failure in the clot formation. Later on, liquefaction of clot occurs and cause bone marrow necrosis. This results in trabecular resorption by osteoclastic activity. The occurrence of lesion in mandible and in young individuals is supported by minor trauma theory which effects hemopoietic marrow.1, 4, 7, 8 A simple bone cyst is usually asymptomatic and discovered accidentally on routine radiography. Sometimes, symptoms have been reported which includes swelling, pain, pathologic fracture, etc.4, 7, 9 Radiographically, the cyst appears to be radiolucent and mostly with well-defined borders. Scalloped margins may be seen where they extend between the roots of the involved teeth, which is the characteristic feature of SBC.4, 8, 10 SBC can be solitary or multiple, and they may also be associated with other pathologies like apical periodontitis, cemento-osseous dysplasia or fibrous dysplasia and cementoma.5, 9, 11 Surgical management is the treatment of choice for SBC. Curettage of the bone walls, can lead to healing of the lesion. Recurrences are rare, and may occur within three months of surgery.12
Case Report
An 18-year-old male patient reported with pain in the right lower back teeth region for 2-3 days. Pain was sudden, throbbing, and intermittent. There was no history of fever, swelling or relevant medical and family history. Provisional diagnosis considered were decayed 47 with apical periodontitis, and pericoronitis associated with 48. Orthopantomograph showed solitary radiolucency periradicular to 48 and 47 region and decay in 46,47 alongwith widening of periodontal ligament space in 47. Rdaiographic findings were suggestive of radicular cyst in relation to 47 and differential diagnosis of benign odontogenic tumor, odontogenic keratocyst and simple bone cyst were considered. (Figure 1) A cone-beam computed tomography (CBCT) scan showed a non expansile solitary hypodensity with defined margin on the right side of the mandible. The lesion extended antero-posteriorly from retromolar region of 48 till the mesial root of 47, and superio- inferiorly from alveolar crest to inferior border of the mandible. The greatest measurement of the lesion was approximately 16.8 mm x 24.63 mm. Scalloped border was visible at the interdental region extending to alveolar crestal bone which is considered as radiographic feature for SBC.(Figure 2) Aspiration was negative. Biopsy was planned. The surgical site was cleaned and sterilised with an antiseptic solution while the patient was placed comfortably in a reclined position. Inferior alveolar, lingual and buccal nerve block was administered with 2% lignocaine and 1: 100000 adrenaline as vasoconstrictor. Prognosis of the 47 appeared poor due to gross destruction of the crown structure as seen in CBCT. Thus, to achieve proper access, flap resection was done followed by extraction of 47 and 48. Lesion was surgically approached through alveolar process. An empty cavity was found with a friable lining which suggested diagnosis of SBC. The lesion was irrigated with a sterile saline solution. Curettage of the cavity was done and fresh bleeding was induced. It was carefully performed to avoid damage to the inferior nerve and vessels. Then the cavity was sutured with 3.0 silk thread reverse cutting, 16 mm needle. Postoperative medication was prescribed for 05 days and included amoxicillin with clavulanic acid 625 mg thrice a day, Diclofenac 50 mg twice a day for analgesia. The histopathological report was suggestive of a non-specific inflammatory reaction. Correlating clinical, radiological and histopathological findings, a diagnosis of SBC was made. To prevent antagonist movement removable prosthesis was advised for the time being and followed by implant placement was planned.(Figure 3) Four month follow up was uneventful and radiograph showed satisfactory bone healing with no recurrence.
Figure 1
A): Showing 46, 47 decayed and pericoronitis in relation to 48. B): Radiograph with arrow showing periradicular hypodensity around 47, 48 root
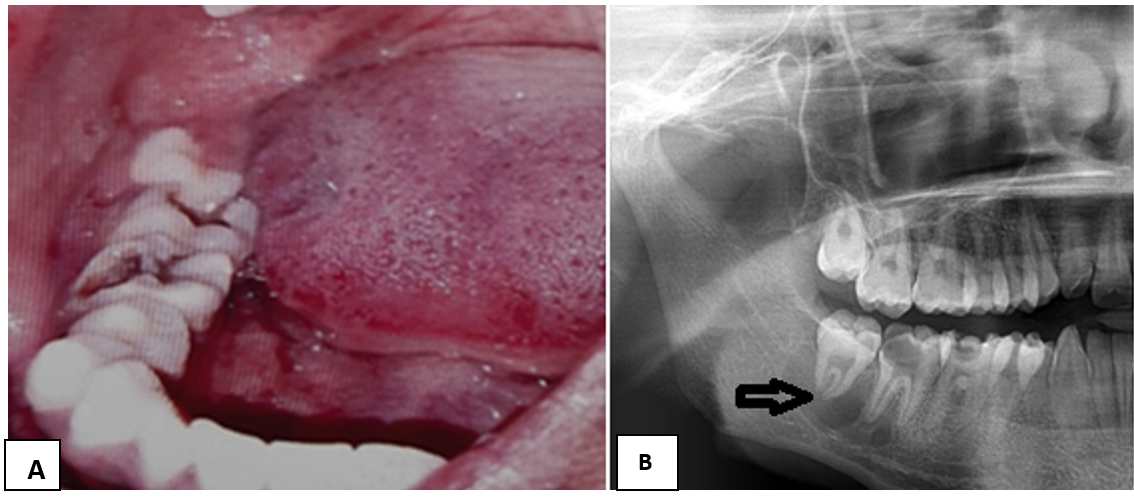
Figure 2
A,B,C,D,E): CBCT scan showing a well defined hypodense lesion in mandibular body (47 and 48 region). Black arrowhead in 2C showing thin buccal wall of decayed 47. White arrowhead in 2E showing scalloped border interdentally
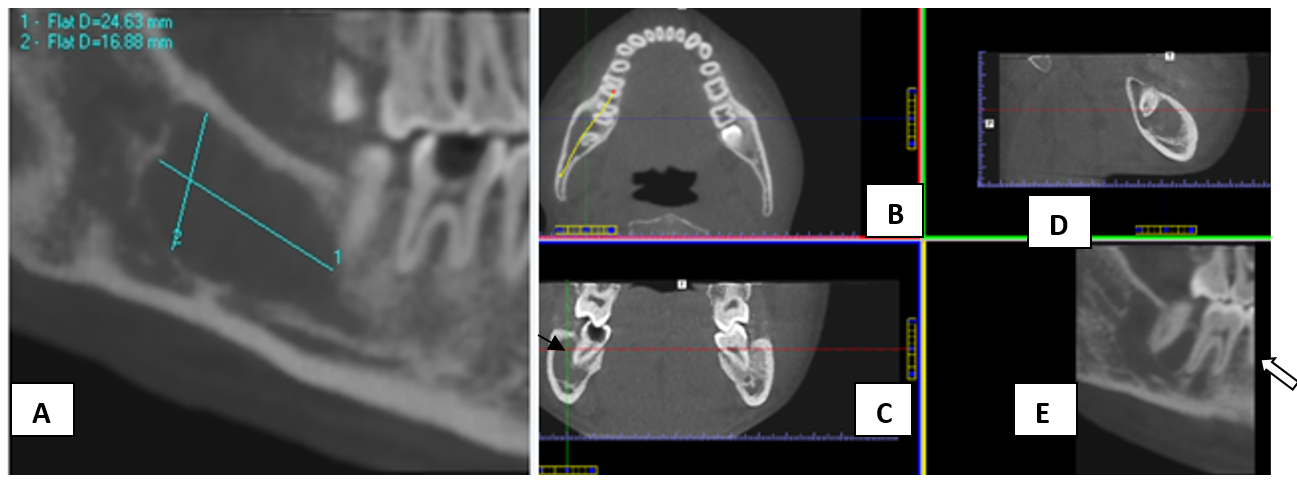
Figure 3
Radiographic evaluation of operative site after 04 months shows decrease in hypodensity with trabecular bone

Table 1
Summarizes few reported case/case series of solitary bone cyst
|
Author and year of publication |
Age/Sex |
Number of patients |
Clinical features |
Radiographic features |
Treatment |
|
Lima LB et al.4 2020 |
30 males and 30 females |
60 cases |
81% asymptomatic 16.6% pain or swelling 1.7% bot pain and swelling |
Mostly radiolucent solitary lesions and Multiple lesions in 2 patients. Expansile in 5 cases, displaced mandibular canal in 3 cases, |
Most cases treated by surgical exploration and curettage. |
|
Dhopte A et al13 2022 |
20yrs/M |
01 |
Incidental finding on panoramic view. |
Unilocular cyst like lesion of mandible in panoramic view and CT scan. |
Curettage and bone graft placement. |
|
Pérez-Iglesias B et al,3 2021 |
16yrs/M |
01 |
Incidental finding on Panoramic radiograph. |
Mandibular angle and ascending ramus. Unilocular radiolucent, size 3x2.5cm with cortical expansion. |
Empty cavity, curettage performed. |
|
Kojima I et al,14 2020 |
39 yrs/F |
01 |
Incidental finding on Panoramic radiograph. |
CT scan Unilocular, scalloped hypodense lesion of mandible Hyperintense signal on fat suppressed T2 MRI images. |
Surgical management. Cemento-osseous dysplasia with small bone cyst. |
|
Musu D et al,5 2020 |
27 yrs/M |
01 |
Incidental finding on panoramic radiograph. |
CBCT showed unilocular lesion with mild lingual expansion. |
Serum /blood fluid evacuated followed by curettage. |
|
Bindra S et al,1 2019 |
25yrs/F |
01 |
Incidental finding on radiograph. |
03 SBC lesion in mandible -2 unilocular and 01 multilocular. Displaced IAC. |
Empty cavity with scarce amount of soft tissue. |
|
Brunet Lobet L et al,9 2019 |
15yrs/F |
01 |
Incidental finding on a panoramic radiograph. |
Unilocular lesion with thinning of lingual cortical bone. |
Serohematic fluid drained by Cannulation. |
|
Matsuda et al.,6 2019 |
13yrs/M |
01 |
Painless swelling with facial asymmetry from 1.5 years. |
CT and OPG: Unilocular expansile radiolucent lesion, premolar to mandibular ramus, 70x30 mm. The mandibular canal could not be confirmed. MRI demonstrated high signal intensity including linear low signal area, which was considered an inferior alveolar nerve on the T2‑weighted image |
Serous fluid with floating neurovascular bundle confirmed with endoscopy. |
|
Patil SP et al,7 2019 |
15 yrs/F |
01 |
Incidental finding on CBCT scan planned for implant placement. |
OPG and CBCT findings: Unilocular lesion of right posterior maxilla with scalloped margin. |
Thin red color aspirate. Incisional biopsy showed scanty fibrous tissue. |
|
Martins Filoh PRS et al,15 2012 |
17 male and 9 female |
26 |
Most patients were asymptomatic |
Radiographically 19 cases were unilocular and 07 cases were multilocular. |
70% cases were filled with air and rest with serous fluid with blood or only blood. |
Discussion
SBC commonly occurs in the metaphysis of long bones like humerus (65%) and femur (25%).6, 9 Only 1% of the lesion occurs in the orofacial region. In orofacial region, it commonly occurs in the mandible; in the premolar- molar region, followed by the ramus and midline of mandible.1, 9 The maxillary lesion is rare and may occur in anterior maxilla or posterior maxilla.1, 7 This lesion is more prevalent in younger age group, usually in the second decade of life, as seen in our case. Male to female ratio is slightly higher or an equal ratio to male ratio.7 It is a solitary lesion which is usually asymptomatic and less than 3cm in size but can also be multiple. Multiple cystic lesions are common in older females and in the maxillary region. Coexistence of other pathologies with SBC has been reported in some cases which include cementosseous dysplasia, apical periodontitis, and cementoma. Radiographically it is mostly unilocular and rarely multilocular with well defined borders; scalloped margins may extend among dental roots and usually. Uncommonly few cases have shown cortical expansion, thinning of cortical lining, root resorption or tooth displacement.4, 7, 12
Long lasting lesions may report with complaint of pain (10-30%) and buccal expansion (18-50%).10 Lesion is usually present above the mandibular canal, but in some cases, displacement of the canal may be seen.6 Surgical exploration may show either empty cavity, serous bloody fluid, serous fluid, shreds of necrotic blood; without an epithelial lining.12, 16 The analysis of the fluid content of the cyst shows high cholesterol and low protein content.1, 3, 16 Curettage is considered as treatment of choice for SBC, which induces bleeding and facilitates osteogenesis in the cavity. Protein rich- plasma protein and autologous bone grafting can also used for bone regeneration.3, 6
The recurrence rate of SBC is low and it usually occurs within three months of surgery. High recurrence rate were seen in cases of 71% cases of multiple cysts and 75% of cases with florid cemento-osseous dysplasia.12 Suei et al. suggested an association between recurrence with radiographic features of absent lamina dura, scalloped margins, bone expansion, radiopaque mass, and multiple cavities.6 SBC should be treated early as a large cystic cavity may cause pathologic fractures and usually simple curettage is sufficient to promote osteogenesis. Floating mandibular nerve has been reported in one SBC case report lesion which was confirmed by endoscopic examination. In our case, the margins of the mandibular canal were indistinct within the lesion, on CBCT which could be one of the radiographic presentations for freely placed mandibular nerve within the canal. As a precaution, the surgeons should consider the possibility of finding floating nerve bundles within the cavity and should not damage the nerve.6, 12 Follow up of 14 cases showed no relapse after conservative surgical treatment. Thus, as a precaution aggressive treatment must be avoided to preserve noble structures like nerves in affected areas.4
Conclusion
Solitary bone cyst is an uncommon occurrence in jaws. Majority of these lesions may not be reported by patients because of its asymptomatic nature and usually diagnosed incidentally. To ensure correct diagnosis and treatment, adequate knowledge about the clinical, radiological and histopathological nature of the lesion should be known to the clinician. Radiographic presentation of scalloped, unilocular or multilocular lesion should include solitary bone cyst as differential diagnosis. Post operative follow up of the lesion is recommended to rule out recurrence of the lesion. Simple bone cyst usually has a much fairer prognosis and responds well with surgical management.
