- Visibility 80 Views
- Downloads 7 Downloads
- DOI 10.18231/j.jooo.2024.056
-
CrossMark
- Citation
Basal cell carcinoma: A report of a case in the upper lip
Introduction
Basal cell carcinoma (BCC) is a malignant epithelial tumor that develops from the basal cell layer of the epidermis. According to the American Cancer Society (ACS), skin cancer is the most common form of cancer,[1] with BCC being the most frequent type.[2], [3], [4], [5]
BCC is classified as a non-melanoma skin cancer along with squamous cell carcinoma.[6], [7] It is mostly found on the head and neck regions and more frequently seen in older adults, with the highest occurrence in people aged 40 to 79.[4], [5] This form of cancer rarely metastasizes but is known to be locally invasive.[8], [9], [10] The most prevalent risk factors for BCC include psoralen, occupational activity, and ultraviolet (UV) radiation exposure.[4], [11]
The lesion presents as a rough, red patch or plaque-raised bump on areas of the skin exposed to the sun.[12] It starts as a firm, painless papule that slowly grows and a central depression takes place, with arborizing blood vessels in the rolled border. In some cases, a central ulceration develops, and this area often experiences intermittent bleeding followed by healing.[5] The expansion of this lesion often destroys underlying structures, arriving at the bone.[13]
Many different subtypes of BCC have been described; the majority of them fall into four main clinicopathologic categories: nodular, superficial, morpheaform, and fibroepithelial, with the nodular (noduloulcerative) being the most frequent.[14], [15] A delayed diagnosis of BCC might lead to a worse prognosis because of its resemblance to eczema, psoriasis, tinea corporis (ringworm), and actinic keratosis. Therefore, prompt identification and therapy are necessary for its efficient management.[1]
BCC can be managed surgically; non-surgical approaches such as radiation therapy, topical treatments like imiquimod and fluorouracil cream, and photodynamic therapy have been proposed.[7], [12], [15]
In this report, we describe a rare case of BCC in the upper lip of a 43-year-old male.
Case Presentation
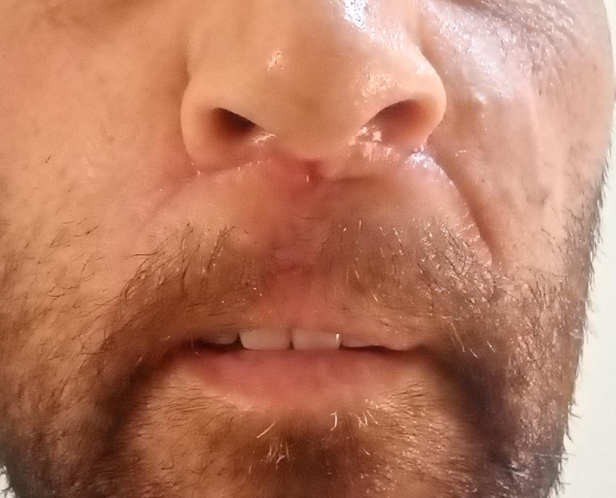
A 43-year-old male, employed in aluminum production and installation, presented to our clinic with a swelling on his upper lip dating four months back ([Figure 1]).

Medical and physical examinations revealed a healthy man with no extra-oral abnormal findings. The patient was a former smoker for 10 years, having quit one year prior. He reported no personal or family history of skin cancer. He had initially noticed a small, painless lump on his upper lip, just under the nose. Two months later, he noticed the lump appeared to have migrated to a lower position towards his lip. The patient consulted an otolaryngologist who, without performing any diagnostic tests (according to the patient), incised and compressed the lump, resulting in fluid drainage. Following this intervention, the lump increased in size and became gradually firmer. Upon presentation to our clinic, clinical examination revealed an 8mm firm and immobile nodule on the upper lip.
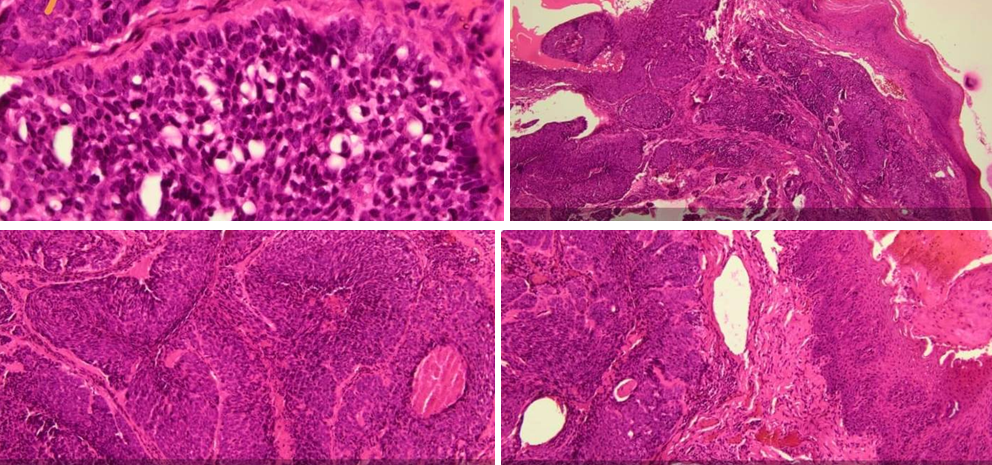
An ultrasound was ordered and demonstrated diffuse calcifications within the nodule. An incisional biopsy was performed, and histopathological examination revealed neoplastic proliferation consisting of infiltrating basaloid cells arranged in trabeculae. The diagnosis was in favor of a BCC ([Figure 2]).
An MRI was performed to assess for bone involvement, which was not detected. Afterwards, the patient was referred to a maxillofacial surgeon who excised the lesion along with surrounding tissue to ensure clear margins. The specimen was sent for second histopathological examination, which confirms the diagnosis of BCC. A routine follow-up examination was carried out after 2 weeks ([Figure 3]).
Discussion
Most BCC cases affect individuals aged 40 and above, and the incidence rate increases significantly with age, particularly among those between the ages of 70 and 75, who make up the largest demographic for BCC diagnoses.[4], [16], [17] A notable feature of this case is the patient's relatively young age of 43, which is uncommon for typical BCC demographics.
BCC is the most prevalent cancer on the cutaneous surfaces of the head and neck regions, a highly sun-exposed area (80% of the cases).[4], [10] In this instance, the BCC is on the upper lip, which is consistent with the common areas for BCC occurrence as on the head and neck.
As for risk factors, they include age, male sex, race, phenotypic characteristics, and genetic predisposition. These factors may interact with environmental exposures, such as UV light or iatrogenic exposures.[18] Our patient's outdoor work significantly heightens the risk of BCC, as epidemiological studies suggest outdoor workers are at a much higher risk of developing the condition due to prolonged sun exposure.[18] Additionally, the patient’s occupational exposure to potential carcinogens[4] and a history of smoking are relevant risk factors. While current smoking may be associated with a lower risk of BCC compared to never smokers, the patient's history of smoking adds complexity to the risk assessment, as this relationship is influenced by detection bias and overall health behaviors, requiring further research.[19], [20] The patient also lives in an area where psoralen, a known risk factor for BCC, is common, thus increasing the likelihood of exposure.[5] Chronic arsenic exposures is a known risk factor for BCC. While its medical use is now limited to treating certain hematological cancers, arsenic can still be found in some work environments, such as in industry and agriculture, two domains central to our patient's life.[21]
Proper diagnostic procedures, such as biopsies and imaging, are essential in confirming a diagnosis of BCC and in distinguishing it from other conditions that may appear similar and determining the most effective treatment plan. Biopsy, which is considered the gold standard for diagnosing BCC, allows pathologists to determine the specific subtype of BCC, which can inform prognosis and treatment decisions.[22] The histological features of BCC include a tumor originating from the surface of the epithelium, scattered mitotic figures and apoptotic cells, the presence of mucoid ground substance, and a tumor infiltrating extensively throughout the connective tissue and often exhibiting a noticeable retraction artifact.[23]
Imaging techniques, such as ultrasound or MRI, may be used in some cases to assess the extent of the tumor, particularly for larger or more aggressive BCCs.[21] This information can help guide surgical planning and ensure complete removal of the tumor. In our case, an ultrasound was performed after clinical assessment; there were signs of calcification in the lesion. A small number of BCC cases show calcium deposits linked to BCC-related keratin, necrosis, or tumor regression.[24] Similar to other follicular-derived tumors, BCC keratins are prone to calcification. These calcium deposits can also be found in the dermis, especially in sun-damaged skin, serving as a histological indicator of BCC in the surrounding tissue.[25] Moreover, we performed an MRI to make sure the damage is local to the skin and not affecting the bone, as BCC is known to be locally invasive.[8], [9] The damage was limited to the skin in our case.
In the context of BCC treatment, surgical intervention, particularly Mohs micrographic surgery, is considered the gold standard due to its precision and high cure rates.[6] For low-risk or superficial BCCs, destructive methods such as curettage, electrodesiccation, and cryotherapy offer viable alternatives.[6] Non-surgical options include photodynamic therapy and topical medications like 5-fluorouracil and imiquimod, which have shown efficacy in treating superficial subtypes.[15] Radiotherapy may be considered in specific clinical scenarios, such as advanced or metastatic BCCs. [9], [12] Treatment selection requires comprehensive evaluation of patient factors, tumor characteristics, and available resources to tailor the most appropriate strategy. Several published guidelines suggest clinical margins for BCC excisions, recommending 3 to 5 mm of uninvolved skin, with the excision depth reaching the mid-subcutaneous adipose tissue. [22] However, these margins may not always be practical in areas like the face, where functional limitations or cosmetic concerns are more significant. In our case, the patient lost some of his lip elasticity, leading to a limitation in his mouth opening because of the amount of tissue excised.
Following a BCC diagnosis, a full-body skin examination is recommended 1 to 2 times per year, adjusting the frequency based on any new skin cancer diagnoses. More frequent exams are advised for high-risk patients or those with high-risk tumors.[15] The recurrence rate for BCC after surgery is typically low, ranging from 1.3% to 10% over five years, influenced by factors like tumor type and patient characteristics. [22], [26]
Conclusion
BCC is a common type of skin cancer of the head and neck regions. Due to its challenging diagnosis, biopsy and prompt identification are essential to making a correct diagnosis and applying the correct treatment.
Source of Funding
None.
Conflict of Interest
None.
References
- P Gruber, P M Zito. Skin Cancer. StatPearls [Internet 2023. [Google Scholar]
- A Lomas, J Leonardi-Bee, F Bath-Hextall. A systematic review of worldwide incidence of nonmelanoma skin cancer. Br J Dermatol 2012. [Google Scholar]
- M Ciążyńska, G Kamińska-Winciorek, D Lange, B Lewandowski, A Reich, M Sławińska. The incidence and clinical analysis of non‑melanoma skin cancer. Sci Rep 2021. [Google Scholar]
- FJ Bath-Hextall, W Perkins, J Bong, HC Williams. Interventions for basal cell carcinoma of the skin. Cochrane Database Syst Rev 2007. [Google Scholar]
- BW Neville, DD Damm, CM Allen, AC Chi. . Oral and maxillofacial pathology 2016. [Google Scholar]
- LA Kwasniak, J Garcia-Zuazaga. Basal cell carcinoma: evidence-based medicine and review of treatment modalities. Int J Dermatol 2011. [Google Scholar]
- DP Kim, KJB Kus, E Ruiz. Basal cell carcinoma review. Hematol Oncol Clin North Am 2019. [Google Scholar]
- NT Huynh, MJ Veness. Basal cell carcinoma of the lip treated with radiotherapy. Australas J Dermatol 2002. [Google Scholar]
- R Kudchadkar, K Lewis, R Gonzalez. Advances in the treatment of Basal cell carcinoma: Hedgehog inhibitors. Semin Oncol 2012. [Google Scholar]
- A Cojocaru, EA Marinescu, O Nica, E Ilinoiu, A Negrila, ME Ciurea. Basal cell carcinoma and its impact on different anatomical regions. Curr Health Sci J 2021. [Google Scholar]
- Z Hallaji, H Rahimi, M Mirshams-Shahshahani. Comparison of risk factors of single basal cell carcinoma with multiple basal cell carcinomas. Indian J Dermatol 2011. [Google Scholar]
- EH Epstein. Basal cell carcinomas: attack of the hedgehog. Nat Rev Cancer 2008. [Google Scholar]
- SL Gillanders, A Mchugh, J Hintze, MJ Donnelly. Erosive rodent ulcer of the ear secondary to neglect. BMJ Case Rep 2020. [Google Scholar]
- TR Wade, AB Ackerman. The many faces of basal-cell carcinoma. J Dermatol Surg Oncol 1978. [Google Scholar]
- MS Heath, A Bar. Basal Cell Carcinoma. Dermatol Clin 2023. [Google Scholar]
- F Al-Qarqaz, M Marji, K Bodoor, R Almomani, WA Gargaz, D Alshiyab. Clinical and demographic features of basal cell carcinoma in North Jordan. J Skin Cancer 2018. [Google Scholar]
- M Ciążyńska, J Narbutt, A Woźniacka, A Lesiak. Trends in basal cell carcinoma incidence rates: a 16-year retrospective study of a population in central Poland. Postepy Dermatol Alergol 2018. [Google Scholar]
- A Bauer, TL Diepgen, J Schmitt. Is occupational solar ultraviolet irradiation a relevant risk factor for basal cell carcinoma? a systematic review and meta-analysis of the epidemiological literature. Br J Dermatol 2011. [Google Scholar]
- A Arafa, A Mostafa, AA Navarini, JY Dong. The association between smoking and risk of skin cancer: a meta-analysis of cohort studies. Cancer Causes Control 2020. [Google Scholar]
- JC Dusingize, CM Olsen, NP Pandeya, P Subramaniam, BS Thompson, RE Neale. Cigarette smoking and the risks of basal cell carcinoma and squamous cell carcinoma. J Invest Dermatol 2017. [Google Scholar]
- E Dika, F Scarfì, M Ferracin, E Broseghini, E Marcelli, B Bortolani. Basal cell carcinoma: a comprehensive review. Int J Mol Sci 2020. [Google Scholar]
- K Uhlman, M Bonert, K Yuen, F Farrokhyar, A Thoma. Margin status of basal cell carcinoma: What can be done better?. J Plast Reconstr Aesthet Surg 2024. [Google Scholar]
- TR Woods, DM Cohen, MN Islam, FJ Kratochvil, JC Stewart, SL Reeder. Intraoral basal cell carcinoma, a rare neoplasm: report of three new cases with literature review. Head Neck Pathol 2014. [Google Scholar]
- EA Slodkowska, B Cribier, B Peltre, DM Jones, JA Carlson. Calcifications associated with basal cell carcinoma: prevalence, characteristics, and correlations. Am J Dermatopathol 2010. [Google Scholar]
- A Tomás-Velázquez, O Sanmartin-Jiménez, JR Garcés, MA Rodríguez-Prieto, V Ruiz-Salas, ED Eusebio-Murillo. Risk Factors and Rate of Recurrence after Mohs Surgery in Basal Cell and Squamous Cell Carcinomas: A Nationwide Prospective Cohort (REGESMOHS, Spanish Registry of Mohs Surgery). Acta Derm Venereol 2021. [Google Scholar]
- A Hasan, A Rabie, M Elhussiny, M Nasr, MI Kamel, A Hegab. Recurrent cutaneous basal cell carcinoma after surgical excision: a retrospective clinicopathological study. Ann Med Surg (Lond) 2022. [Google Scholar]
